Current epidemiological studies estimate that approximately 1% of the world's population could be diagnosed with autism. Several studies have demonstrated that autism has a strong genetic basis, and more than 200 genes have been associated with the condition. Current challenges include both improving early diagnosis and offering support or care pathways, where necessary, that take account of each individual's aptitudes and difficulties.
History
Autism was first described by psychiatrists Leo Kanner in 1943 and Hans Asperger in 1944. Since then, the definition and diagnostic criteria of autism have evolved, and knowledge is growing about the biological – primarily genetic – mechanisms involved. In the 1980s, British psychiatrist Lorna Wing rejected the idea that autism is a binary condition (either present or absent) and suggested that it is more akin to a series of symptoms whose intensity can be situated on a continuum. For example, if we consider social communication impairments, these may vary from difficulties establishing interactions with others to severe social withdrawal. Based on this new approach, Lorna Wing suggested that autism occurs more frequently than initially thought.
Causes
For most autistic people, a medical examination reveals no single cause of the condition. A number of environmental factors have been identified, including neuroinflammation, viruses, and administration of certain drugs (such as sodium valproate) during pregnancy. However, vaccines, celiac disease and parental psychological characteristics are not risk factors for autism in children. The main contributing factor is genetic; in some cases a single de novo mutation (or DNM – a mutation that is absent in the parents and first appears in the child) is responsible for autism. In other cases, a combination of several genetic variations increases the risk of developing autism. Two hundred genes are currently associated with autism, with new genes regularly identified. Studies have also revealed that a significant proportion of the genetic variations associated with autism are shared by other conditions such as attention deficit disorder, with or without hyperactivity (ADD/ADHD), and intellectual disability.
Epidemiology
Depending on the definition applied, the global prevalence of neurodevelopmental disorders is between 5 and 15%, with impairments ranging considerably in terms of severity. According to official data, over 1 in every 100 individuals could potentially be diagnosed with autism. For reasons that are not yet fully understood, boys are more commonly diagnosed with autism (4 boys to every 1 girl). Recent studies have sought to gain insights into how autism is expressed and also the difference in autism diagnosis rates in girls and women. The probability of having a child with autism is 10 to 20 times higher in families where the parents already have an autistic child. Monozygotic twins ("identical twins") are also more likely to share an autism diagnosis than dizygotic twins ("fraternal twins").
Classification
The benchmark classifications (ICD and DSM) and diagnosis of autism are constantly evolving. The condition is now included in the broad category of neurodevelopmental disorders, like attention deficit disorder (with or without hyperactivity – ADD/ADHD), intellectual disability, developmental coordination disorder or specific learning disorder. Neurodevelopment refers to all the mechanisms that guide the way in which the brain develops, orchestrating the brain's functions (motor, executive, sensory integration, language, emotional, reasoning, etc.). It is a dynamic process influenced by genetic and environmental factors. Neurodevelopment begins very early on, before birth, and continues until adulthood. This process of maturation changes the child's capacities on a daily basis. Its speed varies among individuals. These developmental processes may exhibit a degree of diversity, in some cases leading to a neurodevelopmental disorder.
Diagnosis
Diagnosis of autism is clinical. It is based on a precise, detailed, tailored multidimensional assessment that considers various developmental and functional aspects and also the individual's environment in a variety of contexts.
This assessment is based on a coordinated approach involving the individual, his/her family and any professionals involved, and is used to draw up a tailored support plan. It is based on:
- gathered using questionnaires completed by the individual's family, especially the parents where possible, but also professionals that the individual encounters on a daily basis, for example at nursery or school, or in the workplace for older individuals.
- standardized tests (for language, motor skills, etc.) that are appropriate for the individual's age, development profile and behavior and for the context in which the test is being performed. Recognized tests and scales (e.g. those recommended by the French National Authority for Health) should be used if possible.
The importance of autistic individuals' perceptual functioning and thought patterns, whose idiosyncrasies have been widely researched, should be taken into account.
Symptoms
Any autistic individual may present at any age with some or all of the common symptoms set out in this non-exhaustive list:
- limited areas of activity/interest
- difficulties with social integration (social withdrawal or conversely some or even significant effort made to interact socially, although in a way that is considered inappropriate)
- impaired non-verbal communication (e.g. avoiding eye contact)
- difficulty understanding/identifying other people's feelings
- individuals may be non-verbal, experience language impairment or delay, or conversely, develop language in line with typical milestones or even early (speaking articulately with sophisticated vocabulary, but adopting an "idiosyncratic" style of communication)
- tendency to repeat syllables, words or standard expressions (echolalia)
- repetitive behavior (e.g. rocking, twisting limbs)
- difficulty adapting to changes in routine/environment
- sensory hyper- or hyposensitivity (to sounds, light, smells, tastes, etc.)
Associated disorders
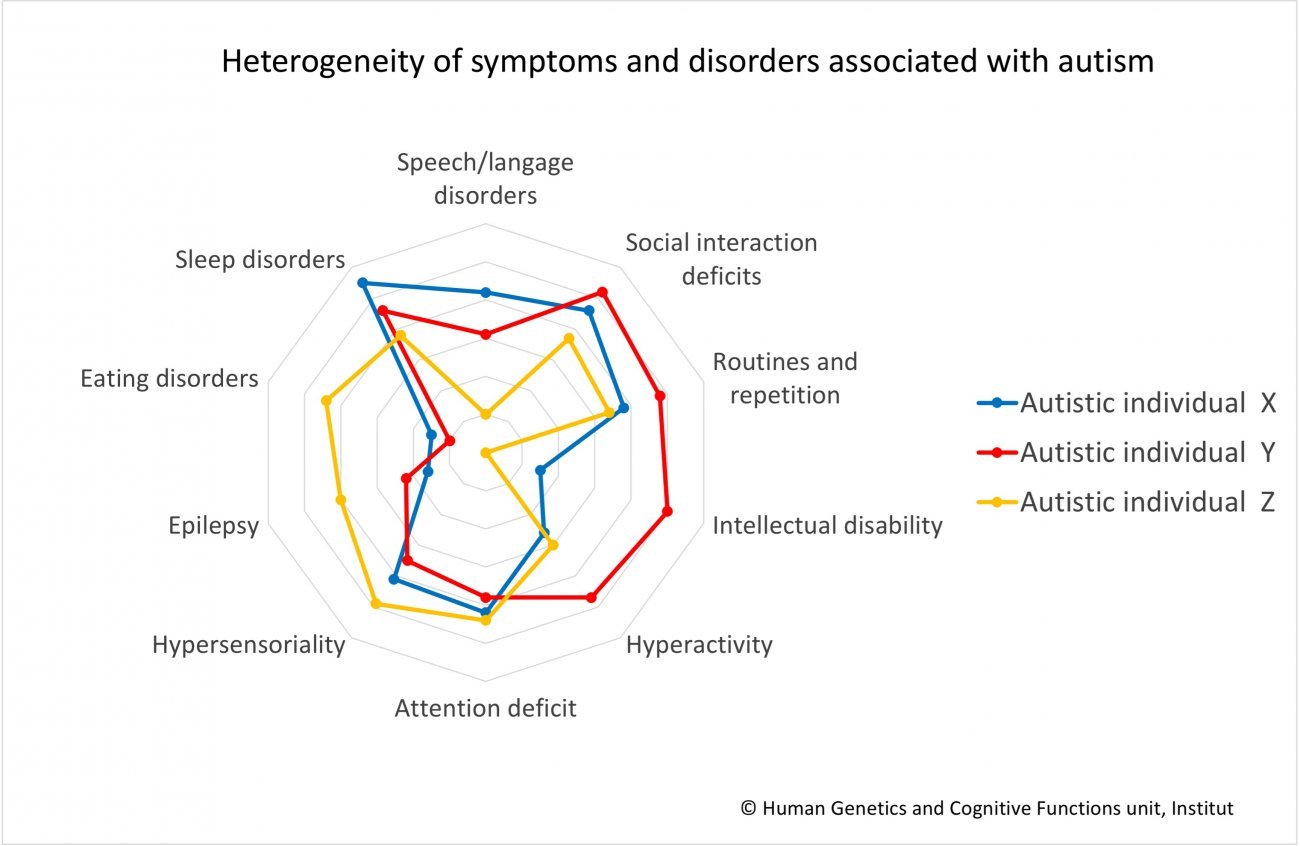
Autism is also frequently associated with other neurodevelopmental disorders such as attention deficit disorder (with or without hyperactivity – ADD/ADHD), developmental coordination disorder, specific learning disorder or intellectual disability, as well as psychiatric difficulties such as anxiety disorder (especially fear of social situations or generalized anxiety disorder), depression, bipolar disorder or even schizophrenic disorder, and other conditions such as epilepsy or gastroesophageal reflux. Autistic individuals also frequently present with sleep and/or eating disorders.
Unfortunately it is only very recently that these associated conditions have been taken into account in research – despite the fact that they are extremely important when it comes to both understanding the origins of autism and improving support for patients.
Approaches and responses
The first priority is to correctly identify signs of autism in anatomical, biological, neurological and clinical terms. Recommendations can then be made to individuals and their families regarding steps to be taken.
Currently, no absolute and exclusive "method" or drug treatment can claim to "cure" autism. However, a combination of educational, cognitive-behavioral and developmental measures has proven to mitigate difficulties, regulate certain states, and enhance individuals' skills. Such steps may be applied to any autistic individual and should be primarily aimed at promoting development and alleviating everyday functional difficulties to improve quality of life.
Treatment of autism is exclusively symptomatic (it treats the symptoms rather than the origins of the disorder) and currently involves tailored non-drug treatment strategies that may include speech therapy, psychoeducation and psychomotor therapy. These strategies are more effective when applied at an early stage of the individual's development. Several therapeutic trials for drug and non-drug treatments are under way to identify other therapeutic strategies.
At the Institut Pasteur
At the Institut Pasteur, the Human Genetics and Cognitive Functions research unit, led by Thomas Bourgeron, a professor at Université de Paris, is engaged in multidisciplinary research drawing on expertise in genetics and structural and functional brain imaging to elucidate the workings of the brain and neurodevelopmental disorders. The unit was the first to confirm the genetic basis of autism when it identified mutations affecting two genes on the X chromosome, NLGN3 and NLGN4X, in 2003. Since then, the team has revealed other genes linked to autism.
The unit's current research is focused on:
- identifying new genes associated with vulnerability to autism and characterizing their particularities;
- incorporating whole genome sequencing and brain imaging data to characterize subgroups of autistic individuals;
- attempting to understand biological mechanisms of autism, including those involved in brain connectivity and melatonin deficiency (linked to sleep disorders which affect over half of all autistic individuals);
- attempting to understand why some individuals are resilient to the severe consequences of certain genetic mutations – in other words they have few or no autistic symptoms despite carrying mutations known to be involved in neurodevelopmental disorders.
Research in collaboration with the InovAND Excellence Center at Robert Debré Hospital
Improving diagnostics
Several projects are being carried out in close collaboration between the Institut Pasteur and the InovAND Excellence Center at Robert Debré Teaching Hospital (part of the Paris Public Hospital Network, or AP-HP), which is led by Professor Richard Delorme. The units in the Child Psychiatry Department hold consultations with families to assess children and develop tailored support programs. Whole genome sequencing is performed by the Genetics Department (Dr. Anne-Claude Tabet). A number of projects are under way to shed light on the recurrence and first signs of autism in young children and the links with identified neuroanatomical and genetic idiosyncrasies. If they wish to do so, the child's parents and siblings can also be assessed in the same department (assessment of medical and psychiatric history, clinical interview and cognitive assessment), to gain insights into how genes associated with autism are passed on within families. A specific project on families with more than one person with autism or neurodevelopmental disorders was recently launched (the "multiplex" families project).
Targeted clinical trials
Although there is currently no drug therapy for individuals with autism or other neurodevelopmental disorders, research suggests that the harmful consequences of some mutations could be reduced, even in adults. In 2022, a clinical trial was initiated at Robert Debré hospital with intellectually disabled autistic individuals carrying SHANK3 gene mutations previously identified at the Institut Pasteur. Using patient skin cells reprogrammed as neurons (induced pluripotent stem cells or iPSCs), Alexandra Benchoua's team at I-STEM performed high-throughput screening of 202 pharmacological molecules and identified a chemical element, lithium, which may restore the level of expression of the SHANK3 gene. The main aim of this randomized clinical trial is to evaluate the effect of 12 weeks of lithium in patients with Phelan-McDermid Syndrome (a form of autism in which the vast majority of patients have a mutation in the SHANK3 gene). Its positive impact on the symptoms of social deficits could represent a new avenue for other syndromic forms of autism. Therapeutic trials with other molecules are under way, especially as part of the European project AIMS-2-Trials (see below).
European research projects: AIMS-2-Trials and CANDY
The AIMS-2-Trials project, funded by the European Union, involves 48 academic and industrial partners. The aim is to identify new biomarkers for autism that will help improve both diagnosis and the development of treatments and tailored support methods. The consortium is conducting therapeutic trials involving various molecules (e.g. arbaclofen).
While the European CANDY project pursues similar objectives to the AIMS-2-Trials project, its scope also includes conditions such as attention deficit disorder (with or without hyperactivity – ADD/ADHD) and epilepsy, which present more commonly in autistic individuals than in the general population. These projects include thousands of participants – newborn infants, children and adults – and monitor their development over several years. The projects involve collecting clinical, genetic and brain imaging data, which will help provide a comprehensive understanding of autism at different levels. This unprecedented volume of research data on autism in Europe should lead to the identification of autistic subgroups and facilitate the discovery of treatments and support tailored to these different subgroups. The Institut Pasteur team is responsible for genetic analyses and for hosting the database for these two projects.
What are the benefits of genetic research for autistic individuals?
Genetic research is beneficial for autistic individuals because it enables:
- A reduction in diagnostic delay. A better understanding of causative genetic mutations will lead to faster, more accurate diagnostics.
- A functional improvement in individuals' everyday lives.Through genome analysis, it is also possible to determine the risk of autistic individuals developing associated disorders, including metabolic disorders, epilepsy and sleep disorders (see insert on sleep disorders in autistic individuals). For example, slow learning caused by certain genes associated with autism and neurodevelopmental disorders may also be mitigated through an appropriate diet, as is the case for patients with metabolic disorders such as phenylketonuria, creatine transporter deficiency and carnitine deficiency.
- Moreover, if mutations causing the disorder in specific individuals can be identified, they can be enrolled in targeted clinical trials assessing the efficacy of a drug treatment and/or educational support for autistic individuals carrying similar mutations.For example, we are currently conducting a clinical trial to test the effect of lithium on reducing symptoms in intellectually disabled autistic individuals with a mutation in the SHANK3 gene (see above "Targeted clinical trials").
The need for participatory research
When researching autism, it has proved important to incorporate clinical, genetic and neurobiological (brain imaging) data, as well as individuals' "experiential knowledge", in other words data related to their real lives. In order to respond to their everyday concerns, needs and also desires, research must imperatively be participatory, with autistic individuals and people involved in their everyday lives given an equal role to scientists and physicians. Several initiatives have been launched, both in France and at European level, enabling stakeholders to collectively identify key areas for improvement in research. Although the number of co-developed research projects is still relatively small, the two major European projects, AIMS-2-Trials and CANDY, each have a dedicated participatory science working group. In particular, the AIMS-2-Trials project issued autistic individuals and carers with questionnaires (in French) to help improve knowledge sharing between scientists and individuals directly affected by autism. In France, the Scientific Interest Group (GIS) on Autism and Neurodevelopmental Disorders set up a think tank for associations of individuals engaged with science (GRAPS). Disabled people are interested and increasingly concerned by issues relating to research. A decision was taken to make co-development a key priority of the Risk, Resilience and Developmental Diversity in Mental Health (R2D2-Mental Health) European project due to start in September 2022, coordinated by the Institut Pasteur Human Genetics and Cognitive Functions unit. The expertise of autistic individuals and their families is crucial for understanding autistic individuals' needs in their everyday lives and improving their well-being.
The contribution of genetics to improving sleep disorders
Sleep disorders have long been clinically identified in autistic individuals. Various studies suggest a correlation between sleep disorders and the severity of autism-specific symptoms and associated disorders.
In 2007, The Institut Pasteur Human Genetics and Cognitive Functions unit, in collaboration with other centers, discovered genetic variations affecting the function of the ASMT gene that encodes the enzyme involved in the synthesis of melatonin (the hormone that regulates biological circadian rhythms). Although low melatonin levels in autistic individuals had already been reported by three independent teams, the cause of the deficiency was unknown. Institut Pasteur scientists observed that over half of autistic children had low levels of melatonin and that this low concentration was correlated with ASMT enzyme deficiency. Educational strategies and melatonin use have since developed to help improve sleep quality and quality of life for autistic individuals and their families.
June 2022
Useful resources
In French:
- Handicap.gouv.fr
- Engagement 1 de la Stratégie Nationale Autisme 2018/2022 consacrée à la Science
- Autisme Info Service
- Groupement National des Centres de Ressources Autisme
- Autisme France
- Autisme Europe
- Deux minutes pour mieux vivre l’autisme
- Comprendre l’autisme
- Association française du Syndrome de Phelan-McDermid
- CléPsy
In English:
This fact sheet was produced jointly with the psychiatric department of Robert Debré Hospital in Paris and the PAARI (People with Autism for Responsible and Innovative Self-Determination) association.

Understanding Autism