Since June 6, 2025, the town of Saint-Quentin (in the Aisne département and the Hauts-de-France region) has witnessed cases of severe food poisoning, mostly in children, caused by Escherichia coli bacteria. We look back at the timeline of events, the epidemiological situation and the Institut Pasteur's role in the crisis.
What exactly is causing the cases of severe gastrointestinal illness that first began to emerge in and around Saint-Quentin on June 6? The health authorities have been working hard between then and now to answer this question. By July 5, 32 cases of food poisoning had been reported in connection with this health alert. Ten of these 32 individuals developed hemolytic uremic syndrome (HUS). This syndrome is characterized by symptoms such as abdominal pain, bloody diarrhea, severe fatigue with pallor, and urinary disorders. The first gastrointestinal symptoms generally appear three to four days after contaminated food has been consumed, though this period can extend to up to ten days in rare cases. HUS causes deterioration of the red blood cells and kidneys, and can lead to death. One young female patient sadly died of it on June 16.
Although some details still need to be clarified, a number of facts have now been established.
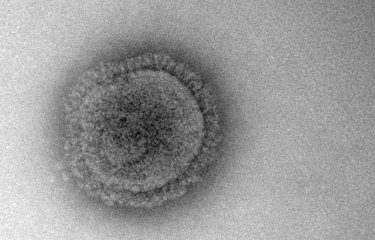
The Escherichia coli bacterium is the cause of these food poisoning cases
• This is bacterial, not viral food poisoning and is caused by the Escherichia coli bacterium. Within this family of bacteria, only those producing a specific toxin (Shiga toxin) and referred to as enterohemorrhagic Escherichia coli (EHEC) cause these severe infections.
• While the pathogen is generally transmitted through contaminated food, human-to-human transmission is also possible through hand contact (hand transmission), highlighting the importance of hygiene measures (hand washing).
• Children, especially those aged under 5, and vulnerable people (the elderly and immunocompromised individuals) are particularly at risk of contracting severe EHEC infections.
The pathogenic bacterium was found in meat, not water
• Tap water, swimming pool water and water from the town of Gauchy was tested and declared safe, thus ruling it out as the source of contamination.
• At this stage of the investigation, the contamination has been traced to meat from certain butchers' stores.
Bacteria detected in certain butchers' stores have been formally linked to those detected in several patients
Bacterial genome sequencing has confirmed that bacteria detected in these butchers' stores (and in meat from these stores) are identical to those detected in patients.
The Institut Pasteur is analyzing bacteria from patients and identifying the responsible bacterium
Additional analyses are also being conducted on other samples. Several aspects of this health alert are still on hold pending a complex epidemiological investigation. This involves a number of stakeholders:
- The Hauts-de-France Regional Health Agency (ARS) and Santé publique France (SpF) are leading the field investigation, which consists of interviews with patients or their families. Their aim is to identify food, places or events that link the various patients, put initial preventive measures in place, and keep the local population updated.
- The Aisne prefecture is responsible for coordinating crisis management at local level and implementing preventive and management measures such as closing butchers' stores.
- The health crisis center of the General Directorate of Health in the French Ministry of Health and Access to Care is responsible for coordinating its regional operators (ARS), the national health agencies (Santé publique France, Institut Pasteur) and interministerial stakeholders, including the General Directorate for Food (DGAl) and the French Agency for Food, Environmental and Occupational Health & Safety (ANSES).
- The legal investigation was first assigned to the public prosecutor for Aisne, before subsequently being referred to the Paris public prosecutor.
- The Laboratory for Investigations of Pathogenic Food-borne Microorganisms/National Reference Laboratory (LMAP/LNR) for Escherichia coli and accredited laboratories are analyzing samples taken by the Departmental Authority for the Protection of Populations (DDPP) and the DGAl at retail outlets/food stores to determine the source of the contaminated food.
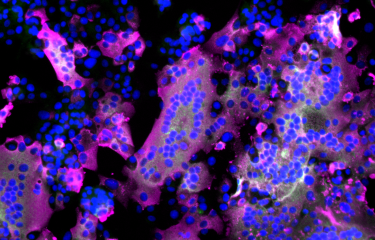
- The National Reference Center for Escherichia coli is analyzing samples taken from patients to confirm the presence of the EHEC bacterium and sequence its genome.
There are two stages to these analyses. The first stage is performed at the associated laboratory for the CNR (at Robert Debré Hospital, Paris). This confirms whether infections are actually caused by EHEC bacteria and isolates the responsible bacterium in each patient to distinguish it from the large number of non-pathogenic strains of Escherichia coli that occur naturally in the human gastrointestinal system. This first phase of the analysis lasts four to six days. The second stage, performed at the Institut Pasteur, involves sequencing the bacterial genome. A bioinformatics analysis is then conducted to determine a genetic profile for these bacteria. This genome analysis enables bacteria taken from patients and those potentially found in food to be compared, thus confirming a causal link between the two. It takes four to five days to prepare for and perform the sequencing and analyze the results.
In a broader sense, efforts to manage these types of food health crises, recent episodes of which include a case of frozen pizzas contaminated with Escherichia coli in 2022, an outbreak of botulism poisoning in September 2023 and the current crisis, hinge on the work of the National Reference Centers (CNRs) involving 19 Institut Pasteur laboratories and close collaboration between the various health authorities.
When the Escherichia coli bacterium causes hemolytic uremic syndromeEscherichia coli is a bacterium that naturally lives in the digestive tract of humans and animals. While most strains are harmless, some have virulence factors and are pathogenic. Which strains of Escherichia coli are dangerous for humans?Enterohemorrhagic Escherichia coli (EHEC) strains give greatest cause for concern. These bacteria contain a gene that encodes the highly potent Shiga toxin, which causes a severe infection known as hemolytic uremic syndrome (HUS). What are the routes of transmission?EHEC is usually transmitted through the consumption of contaminated food (undercooked meat, raw dairy products, contaminated vegetables) or direct contact with animals or carriers. What are the symptoms?While the symptoms of EHEC infection generally appear within three to four days of infection, this period may extend to up to ten days. They include abdominal pain, vomiting, and initially watery then bloody diarrhea. Patients may also experience fever. What are the potential complications?Hemolytic uremic syndrome (HUS) occurs in approximately 5 to 10% of infections, affecting children in particular. It can result in acute kidney failure and other severe conditions one week after the initial gastrointestinal symptoms. How can infection be prevented and what treatments are available?Prevention of EHEC infection requires the application of strict hygiene practices throughout the entire food chain, from producer to consumer. It is essential to wash hands before preparing meals and ensure that food is properly cooked. Most antibiotics are contraindicated, and therefore treatment is focused on managing symptoms and monitoring complications. |