What are the causes?
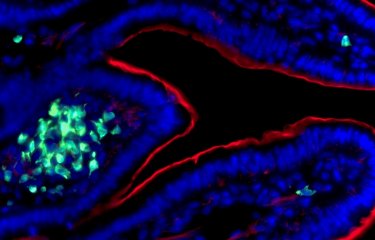
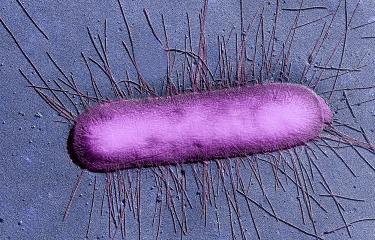
Escherichia coli (E. coli) is a bacterium found in the gut microbiota of humans and animals. Although most strains of E. coli are harmless, some, including EHEC, acquire virulence factors and become pathogenic. They release toxins that generally lead to damage in the vascular endothelium (the layer of cells that lines blood vessels) in the gut and the kidneys.
How do the bacteria spread?
EHEC pathogens are primarily transmitted through the consumption of contaminated food. Since the natural reservoir of EHEC is mainly the digestive tract of cattle, raw or undercooked meat, raw (unpasteurized) dairy products and occasionally raw vegetable products are the main food products affected. Contamination may also occur during the milking or slaughter of cattle. Fecal matter from ruminants found in the earth, in manure or in water (ponds and streams) is another potential source of contamination.
Human-to-human transmission of EHEC is also possible, though rare. In most cases, it is observed in a family environment or in the community (for example in nurseries).
What are the symptoms?
The symptoms associated with EHEC (enterohemorrhagic E. coli) begin 3 to 4 days after infection (source: Anses, 2019). They include abdominal pain and diarrhea, which may develop into bloody diarrhea (hemorrhagic colitis). Vomiting and fever may also occur. Although in most cases the infection clears up by itself, it can sometimes lead to a severe form known as hemolytic uremic syndrome (HUS), which can prove fatal.
How is infection diagnosed?
The best way of detecting E. coli bacteria is a laboratory analysis of the patient's stools. This test confirms the presence or absence of Escherichia coli that cause infection.
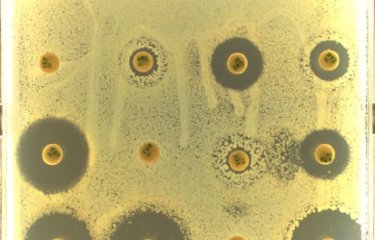
As there are large numbers of Escherichia coli in the digestive tract, laboratory methods are needed to specifically recognize enterohemorrhagic Escherichia coli by detecting the gene encoding Shiga toxin or the toxin itself.
What treatments are available?
Most antibiotics are not recommended for treating EHEC infections. By destroying bacteria, antibiotics trigger the release of Shiga toxins in the body, which can worsen HUS. However, treatments based on certain antibiotics such as azithromycin, which avoid the release of Shiga toxins, are currently being assessed. Pending these results, the therapeutic strategy for HUS involves repairing the damage caused by Shiga toxins, which includes a fall in red blood cell and platelet count and renal impairment, by transfusion, dialysis and plasma exchange.
Episodes of diarrhea are treated symptomatically: patients are rehydrated but are not given anti-diarrheal drugs to ensure that they eliminate the bacterium and its toxins in stools.
How can infection be prevented?
We do not yet have the knowledge needed to reduce the incidence of EHEC on cattle farms. However, tests can be performed to determine whether a given animal carries the bacterium. If necessary, meat can be given bactericidal treatment, which involves heating or irradiation. Although these techniques are useful, they do not systematically guarantee the absence of EHEC in food. Effective prevention of EHEC infection requires the application of strict hygiene practices throughout the entire food chain, from producer to consumer.
People involved in producing and preparing raw vegetable and animal products must be given training in best hygiene practices.
Consumers and cooks can avoid most EHEC infections by adhering to the following guidelines:
- make sure minced beef is cooked right through, especially for children under the age of 5;
- young children should avoid raw (unpasteurized) cheeses;
- wash fruit, vegetables and herbs, especially if they are eaten raw;
- wash your hands before preparing meals and as often as necessary;
- make sure cooking implements are kept clean, especially if they have come into contact with raw meat, to avoid cross-contamination;
- keep cooked and raw food separate;
- do not allow very young children (under the age of 5) to come into contact with farm animals, especially cattle, sheep and their environment;
- do not drink water that has not undergone microbiological testing (from a well or spring).
How many people are affected?
EHEC can be responsible for severe cases of foodborne infection. The first EHEC strain was isolated during a foodborne outbreak in the United States in 1982. The outbreak was caused by hamburgers containing undercooked meat patties. EHEC has since given rise to several other outbreaks and currently represents a major public health issue. Past outbreaks have been caused by contaminated hamburgers, in France in 2005, and fenugreek sprouts, in Europe in 2011.
In France, national surveillance of these infections was introduced in 1996. HUS cases in children aged under 15 are monitored based on reporting from hospital pediatric departments to Santé publique France. In 2019, 71% of pediatric HUS cases were in children under the age of three.
Every year in France there are around 160 severe infections with enterohemorrhagic Escherichia coli.
FAQ
What is Escherichia coli?
Escherichia coli is a bacterium that we have known about for more than a century. The bacterium lives in the digestive tract of animals and humans. There are a huge variety of strains. Most Escherichia coli bacteria live peacefully in the digestive tract, but the evolutionary process has caused some types of bacteria to acquire virulence factors, making them pathogenic for some parts of the body. Two examples:
- the urinary tract (all the organs that eliminate waste from the body), which can be affected by urinary infections;
- the gut, the preferred target of Escherichia coli infections.
Every year in France there are around 160 severe infections with enterohemorrhagic Escherichia coli, resulting in one fatality every year or every other year.
Which Escherichia coli bacteria are dangerous for humans?
At the Institut Pasteur, in the National Reference Center for Escherichia coli, Shigella and Salmonella, we monitor enterohemorrhagic Escherichia coli particularly closely.
These foodborne Escherichia coli have a gene that encodes a highly potent toxin known as Shiga toxin, responsible for a severe infection called hemolytic uremic syndrome (HUS).
Which people are most exposed to Escherichia coli?
The people most at risk from enterohemorrhagic Escherichia coli infections are children, especially very young children under the age of five.
They are more susceptible than others to hemolytic uremic syndrome, which causes the most severe forms of infection.
Which foods can contain enterohemorrhagic Escherichia coli?
Enterohemorrhagic Escherichia coli live in the digestive tract of ruminants. When the animals are slaughtered or milked, contaminated fecal matter can find its way into milk or carcasses. The main foods contaminated with enterohemorrhagic Escherichia coli are therefore:
- minced beef,
- raw (unpasteurized) milk,
- raw milk cheese,
- vegetables that have not been carefully peeled or washed,
- flour-based products.
What is the mode of infection of Escherichia coli bacteria?
Infection with enterohemorrhagic Escherichia coli is generally caused by ingesting contaminated food that is raw or insufficiently cooked. But there are other possible modes of infection, including human-to-human transmission, especially via dirty hands (hand transmission).
There are a higher number of cases in communities involving children – particular care needs to be taken when washing hands after changing the diaper of an infected child to avoid passing the infection on to other people in the same community.
What are the symptoms of Escherichia coli infection?
When food contaminated with enterohemorrhagic Escherichia coli is eaten, the first signs appear after around three or four days, or even up to ten days.
These include abdominal pain, cramps and diarrhea, which can soon develop into bloody diarrhea. One week after these symptoms, a much more severe infection, hemolytic uremic syndrome, may occur. This syndrome occurs in 10% of cases; symptoms include fatigue, pallor and a reduction in urine output, with urine becoming much darker in color.
How can Escherichia coli infection be detected?
Enterohemorrhagic Escherichia coli infection is detected by stool culture performed in the laboratory. This test confirms the presence or absence of Escherichia coli that cause infection.
As there are large numbers of Escherichia coli in the digestive tract, laboratory methods are needed to specifically recognize enterohemorrhagic Escherichia coli by detecting the gene encoding Shiga toxin or the toxin itself.
How can Escherichia coli infection be avoided?
Prevention of enterohemorrhagic Escherichia coli infection is primarily based on good hand hygiene. Hands should be washed thoroughly before preparing meals, after going to the toilet and after touching pets.
When preparing food for very young children, meat should be cooked through, and raw (unpasteurized) milk and soft raw milk cheese should be avoided.
More generally:
- carefully peel and wash vegetables;
- do not eat products made with raw flour (pizza dough or cookie dough);
- do not drink water that has not undergone microbiological testing (from a stream or spring).
How should Escherichia coli infections be treated?
Severe enterohemorrhagic Escherichia coli infections require hospital treatment. The loss of red blood cells (anemia) is treated with blood transfusions and kidney failure is treated with dialysis. Most antibiotics are not recommended: as they destroy the bacteria, they may worsen hemolytic uremic syndrome by releasing greater quantities of toxin.
March 2024