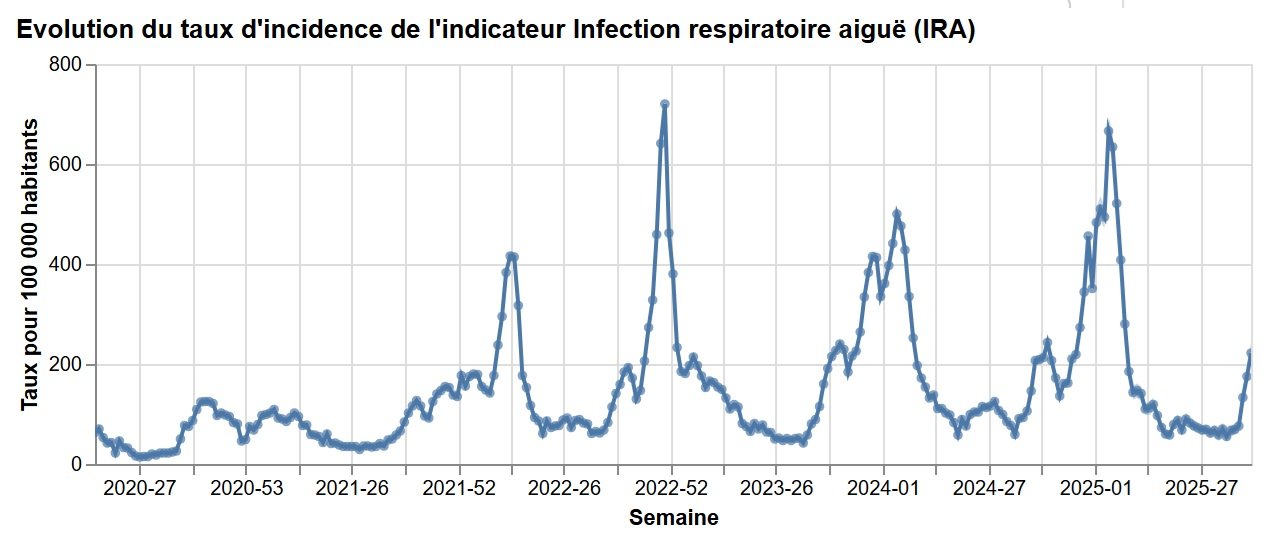
As long as the SARS-CoV-2 virus is still circulating, there is a possibility of new, less intense but persistent waves in France and around the world. In September 2025, the Frankenstein variant, a sub-variant of Omicron with low virulence, was widely observed. So what is the current situation with COVID-19 in France? Interview with Olivier Schwartz, Head of the Virus and Immunity Unit at the Institut Pasteur.
According to Santé publique France, suspected cases of COVID increased by 37% in adults during the week of September 15-21, 2025 in mainland France, down slightly in children, and circulation remains low in French Guiana and the French West Indies. Circulation of SARS-CoV-2 is therefore on the rise, but not at alarming levels. The XFG variant currently circulating is described as more contagious but no more dangerous than its predecessors. It has been dubbed "Frankenstein" because it is a recombination of two sub-variants of the Omicron virus.
SARS-CoV-2 is continuing to circulate, driven by the regular emergence of new variants resulting from mutations that enable it to partially evade immunity. Vaccination and the adoption of hygiene and distancing measures remain essential, particularly for people at risk, and strong global surveillance is needed to prevent the emergence and spread of new variants of concern.
Olivier Schwartz, Head of the Virus and Immunity Unit at the Institut Pasteur, talks to us about the issues raised by the resurgence of suspected COVID cases.

#1. Why does COVID-19 keep emerging in waves at around the same period every year? Will COVID-19 become a strictly seasonal illness, like influenza?
Olivier Schwartz: SARS-CoV-2 is still circulating, with seasonal resurgences similar to those of influenza. So far, the virus has tended to be present in the background all year round, unlike influenza, which is generally seen in winter. As long as there is still partial immunity in the population, the risk is primarily for the most vulnerable individuals.
However, we are seeing a general decline in the number of cases and severe forms of the disease, largely as a result of the immunity acquired through vaccination coverage and past infections.
The persistence of SARS-CoV-2 can be explained by several factors:
- As the virus is constantly mutating, it can partially evade immunity;
- Antibody levels from both infection and vaccination drop over time;
- Winter conditions are conducive to transmission (low temperatures, higher rainfall, windows closed).
#2. How does SARS-CoV-2 mutate? How do these new variants appear?
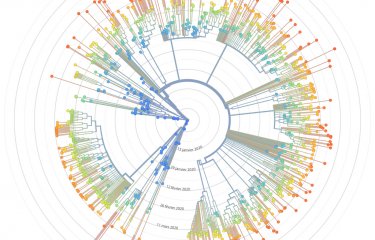
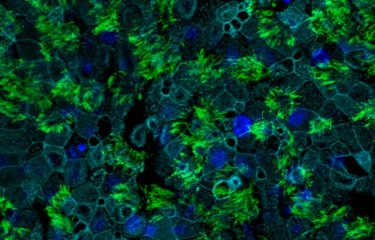
O. S.: Like all RNA viruses, SARS-CoV-2 mutates regularly. Most mutations have no impact or hinder the virus, but a few give it an "advantage," enabling it to spread. The mutations that give rise to what are known as "variants" often occur in the Spike protein (the main target of vaccines and neutralizing antibodies). These variants are generally more capable of infecting cells and bypassing immune defenses.
The most likely scenario is one of "endemicity," where the virus circulates at low levels, sometimes creating small waves. But the emergence of a new, very different variant that is less susceptible to herd immunity cannot be entirely ruled out.
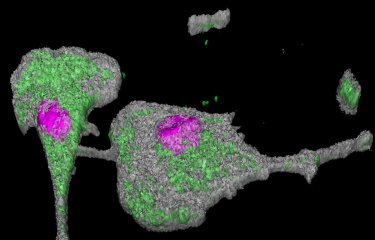
Most mutations occur as the virus circulates, but more virulent variants could emerge in frail or immunocompromised individuals (for example elderly patients or those with severe illnesses or untreated HIV infection), since the virus persists in these people for longer and has time to mutate. That is why it is so important to keep a close eye on these fragile individuals, particularly in developing countries. In the United States, the decline in funding for HIV/AIDS treatment and prevention will lead to an increase in the number people with HIV and could therefore result in a higher risk of new variants emerging (see the article in Le Monde).
The new variants currently circulating, including the Frankenstein variant, are relatively similar in genetic terms. I must say that the name "Frankenstein" seems excessive, as there is currently no evidence to suggest that this virus is any more dangerous than previous variants.
#3. Are the vaccines still effective?
O. S.: Most infections now are less severe, especially in younger people and those with no significant risk factors, in large part because of vaccination or previous infections. Immunity does decline over time, although there is still significant protection against severe forms. That is why it is so important for vaccine composition to be updated regularly, as it is for influenza, and for the most vulnerable populations (over-65s, people with co-morbidities, immunocompromised individuals, etc.) to be given annual boosters. Vaccines adapted to the current variants are available every year.
#4 What are the recommendations for dealing with COVID-19?
O. S.: To weaken the chain of transmission of the virus, as with any respiratory infection, it is important to follow the recommendations issued by health authorities, in particular:
- Isolate as much as possible if you are infected or ill;
- People with risk factors should be (re)vaccinated;
- Air your home, workplace or communal areas regularly;
- Adopt hygiene and distancing measures, especially if you test positive and/or experience symptoms: wash your hands regularly, wear a mask in enclosed spaces, etc.
- Follow the vaccination recommendations issued by health authorities.
Sources :
- Bulletin national d'information OSCOUR du 23 septembre 2025
- Covid-19, cinq ans de l’épidémie : avons-nous retenu les leçons de 2020 ? Revivez notre journée spéciale - Le Monde, 4 mars 2025
- L’épidémie de Covid-19 connaît un regain, sans « aucun signal inquiétant », selon les experts - Le Monde, 3 octobre 2024
- Épidémiologie et conditions de vie sous le Covid-19 : mise en ligne des données des vagues 2020 et 2021 de l’enquête EpiCov | Direction de la recherche, des études, de l'évaluation et des statistiques - Drees, 07 mai 2024