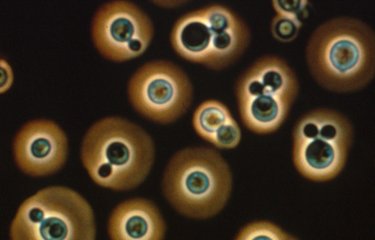
Candidiasis of the skin and mucous membranes
Skin and mucous membrane infections may occur in both healthy and immunocompromised individuals. They are mainly caused by changes in hydration, pH, nutrient concentrations and the microbial environment of the skin and mucous membranes. Several determinants of genetic susceptibility have now been identified for chronic or recurring forms. Candidiasis of the skin develops in high perspiration areas including the groin, armpits, interdigital areas, and on burns or grazes. Candida yeasts may infect various mucous membranes: the oral cavity, the vaginal mucosa and the esophagus.
Thrush is one of the most well-known forms of oral cavity candidiasis, frequently affecting newborns, patients treated with broad-spectrum antibiotics and immunocompromised individuals, especially those with AIDS.
Genital candidiasis or vulvovaginitis is also common and is caused by the species Candida albicans in 80% of cases. These are not classified as sexually transmitted diseases and may indicate diabetes. Relapses may be caused by a number of factors including drugs (repeated courses of antibiotics), estrogens, corticosteroids and immunosuppressants, and contraception by intrauterine device or diaphragm.
Finally, esophageal candidiasis is often associated with HIV infection. Antifungal treatments are required, with treatment length and conditions determined on a case-by-case basis in accordance with international guidelines for which the National Reference Center for Invasive Mycoses & Antifungals is a contributor.
Systemic candidiasis
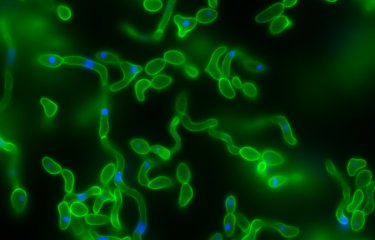
The incidence of systemic candidiasis has increased in France over the past decade. It is caused by two different pathophysiological mechanisms. Firstly, systemic candidiasis may result from "exogenous" nosocomial infections often in patients with intravascular catheters (IV drip products, hand transmission). Secondly, it may occur if yeasts colonizing "endogenous" gastrointestinal and/or genitourinary sites enter the bloodstream and deep organs. Such events are more likely if mucous membranes have been weakened by chemotherapy and long-term antibiotic treatments, mainly in patients admitted to intensive care units, particularly for surgery, but also in neutropenic patients (suffering from a deficiency of neutrophils, a type of white blood cell).
There are multiple risk factors for systemic candidiasis including long-term neutropenia, allogeneic or autologous bone marrow transplant, corticosteroid treatment, major gastrointestinal surgery, intensive care, premature delivery, extensive burns, etc. It can occur in any location, particularly in the kidneys and heart valves.
In epidemiological terms, the species Candida albicans is responsible for approximately half of all infections with all risk factors taken into account. In France, this is followed by Candida glabrata, Candida parapsilosis and Candida tropicalis. The other species are less common and their emergence is often dependent on specific ecologies. If certain species are identified, this may prompt changes to therapeutic treatment due to their intrinsic resistance to certain antifungal agents.
Systemic candidiasis is considered as a potential diagnosis if patients at risk of candidemia present with long-term fever resistant to antibiotic treatments. Diagnosis is confirmed by a positive blood culture. Such cases should be treated systematically with antifungal agents and intravascular catheters should be removed as they are often colonized. Mortality is still approximately 40% and has not fallen despite therapeutic and diagnostic breakthroughs.
June 2021