Cause
Sepsis is the consequence of a severe infection that generally stems from a localized infection (peritonitis, pneumonia, urinary tract infection, catheter-related infection, etc.). It often affects patients with weakened immune systems. When sepsis occurs following an invasive procedure (such as major surgery), the infection is referred to as a nosocomial (or healthcare-associated) infection.
All bacteria, even those naturally present on the skin or in mucous membranes such as the throat, which are normally non-pathogenic, can trigger the onset of sepsis. Fungal infections can also induce a similar response, as can some viruses (such as SARS, SARS-CoV-2 which causes COVID-19, H1N1 influenza and hemorrhagic fevers). Meningococcal meningitis (specifically purpura fulminans) is a rare cause of sepsis that can occur in healthy young people, as is staphylococcal toxic shock syndrome due to tampon use.
History
Throughout history, sepsis has been known by various different names. In the past it was referred to as hospital gangrene (also known as nosocomial fever or putrid fever), a common affliction of soldiers whose war wounds frequently became infected. The most famous example is undoubtedly Richard the Lionheart, who died in 1199 as a result of an infection following an arrow wound. The term puerperal fever was also used to describe infection contracted by women after childbirth. This was how Lucrezia Borgia died in 1519 after giving birth to her seventh child. The French doctor Armand Trousseau was the first to suggest a similarity between nosocomial gangrene and puerperal fever.
In 1847 in Vienna, Hungarian doctor Ignaz Semmelweis showed the importance of hygiene and handwashing in preventing the spread of puerperal fever among women in childbirth. But the contagious nature of puerperal fever had already been suspected by the Scottish doctor Alexander Gordon more than half a century earlier. In 1869, two doctors from Alsace, Victor Feltz (1835-1893) and Léon Coze (1819-1896), first demonstrated the presence of bacteria in the blood of a patient suffering from puerperal fever, a fatal infection subsequently attributed to streptococci. Louis Pasteur, in collaboration with the Port-Royal, Cochin and Lariboisière maternity wards in Paris, confirmed these observations in 1879-1880 and recommended improved hygiene during childbirth.
Symptoms
In 2002, sepsis was defined as a systemic inflammatory response syndrome caused by infection. In 2016 the definition was revised, and sepsis is now defined as a life-threatening organ dysfunction caused by a dysregulated host response to infection, the most severe form of which is septic shock.
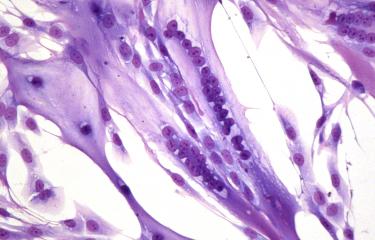
Sepsis is characterized by excessive production of inflammatory mediators, often referred to as a "cytokine storm" because of the overproduction of cytokines (chemical mediators that allow cells to communicate with each other), which have an acute impact on vital organ function and can lead to long-term functional sequelae. Around 25% of sepsis survivors still experience cognitive impairment after more than three months.
Epidemiology
Nowadays sepsis generally affects people at either end of the age spectrum: newborns (neonatal sepsis) or elderly people.
According to the World Health Organization (WHO), sepsis is responsible for one in every five deaths worldwide. There are 49 million cases of sepsis every year, almost half of which occur in children. Around half of patients contract the infection in hospital. In industrialized countries, sepsis is responsible for as many deaths as heart attacks. In developing countries, puerperal sepsis remains a major cause of death for women after childbirth.
In France, there are thought to be around 250,000-300,000 cases of bacterial sepsis each year, as well as cases of fungal and viral sepsis. Some 25% of patients admitted to hospital for sepsis die, and the death rate from septic shock can reach 50%. It is thought that more than 60,000 people die as a result of sepsis every year in France. Estimates suggest that the number of cases may double within the next 50 years, particularly as a result of population aging. In 2017, WHO drew the attention of its member states to the scale of the problem for public health, issuing a resolution encouraging them to improve epidemiological data, preventive strategies, diagnosis and treatment, as well as sepsis research.
Treatment
Patients with sepsis are generally admitted to intensive care, where they are given antibiotics and appropriate support to sustain the body's vital functions.
In over twenty years, despite significant progress in understanding the pathophysiology of sepsis, no new sepsis-specific treatments have emerged. Several costly clinical trials have ended in failure and the only new drug brought to market specifically for this indication (Xigris®) was subsequently withdrawn in 2011 because its efficacy could not be sufficiently proven. There is therefore a real need for novel therapeutic concepts developed on the basis of a more detailed knowledge of the pathophysiological mechanisms involved in sepsis. More rapid diagnostic tests for bacterial sepsis would also allow antibiotics to be administered at an earlier stage. This last point is crucial because every hour gained increases a patient's chance of survival. Recent developments associated with the pandemic caused by the SARS-CoV-2 virus suggest that some treatments used for excessive inflammation caused by viral sepsis (corticosteroid treatment and anti-cytokine monoclonal antibodies) could be beneficial.

New weapons to fight bacteria
September 2021