What are the causes?
The infectious agent responsible for listeriosis is the bacterium Listeria monocytogenes, a 1 to 2 µm-long bacillus that can multiply at low temperatures (4°C). It is a ubiquitous bacterium that can be found in water, soil, plants and the guts of several animals. L. monocytogenes is capable of colonizing food processing environments, meaning that it can cause foodborne infections, especially via contaminated dairy or meat products, and also outbreaks in cases where there has been widespread distribution of contaminated food.
How do the bacteria spread?
The most frequent contamination route in humans is the ingestion of contaminated food. The bacterium is killed by heat, but it can continue to multiply at 4°C (refrigerator temperature). Longer cold chains (industrial cold storage facilities and domestic refrigerators) can therefore lead to food products being contaminated by Listeria monocytogenes. Unlike most other foodborne pathogens, Listeria monocytogenes does not alter the taste of food, which explains why this bacterium may be eaten repeatedly and in large amounts without being noticed.
In France, the food products most commonly contaminated with Listeria monocytogenes are dairy products (especially soft and raw milk cheeses), cooked meat products (tongue, head meat, potted meat products), raw or smoked fish, chilled sprouted seeds, and raw or rare meat.
What are the symptoms?
The incubation period for listeriosis can range from a few days to two months.
There is a non-invasive form of listeriosis, which affects people in good health. It causes non-specific symptoms such as diarrhea, fever, muscle pain and headache.
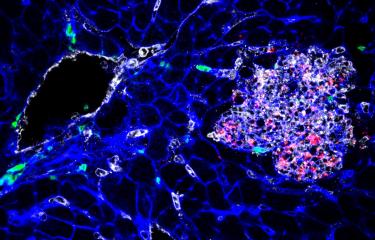
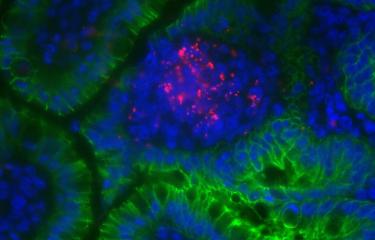
The second form, described as invasive (since the bacteria do not remain in the digestive tract), mainly affects vulnerable and immunocompromised people, like pregnant women, infants, elderly people, people with cancer and transplant recipients. In adults, the disease causes an infection of the blood (septicemia) or even the central nervous system, manifesting mainly as meningoencephalitis (an infection of the membranes, or meninges, covering the brain, and the brain itself).
In pregnant women, the infection is generally benign for the mother. It can even go unnoticed, or may manifest as contractions or fever. But in some cases it may cause miscarriage, preterm delivery or fetal death. Infection is severe in newborns, and often worse in preterm newborns, with symptoms that may include septicemia and infection of the lungs, nervous system and sometimes the skin. Infection in preterm newborns in particular can lead to severe sequelae.
How is infection diagnosed?
Diagnosis is initially based on clinical symptoms. Listeria monocytogenes bacteria can be detected through a blood test or a cerebrospinal fluid sample.
After childbirth, a placental examination can provide valuable information. The first stools of infants can be used for diagnosis.
Bacteriological tests can also be performed on food products suspected of contamination to confirm whether or not they contain Listeria monocytogenes.
What treatments are available?
There is an antibiotic treatment for severe forms. It is taken for several weeks and is more effective if administered rapidly after diagnosis. However, even with targeted early treatment, the outcome may be fatal.
How can infection be prevented?
For at-risk groups (pregnant women, elderly people and people with weakened immune systems due to immunosuppressant drugs or conditions such as cancer, cirrhosis or diabetes), prevention involves avoiding the following foods: dairy products, delicatessen meat products, rillettes, pâté, foie gras, raw milk cheeses, smoked fish, raw shellfish, crab sticks, taramasalata, and raw seed sprouts. The recommendation is to cook all animal products thoroughly, remove all cheese rinds, carefully wash vegetables and herbs, and reheat all ready-to-eat food products to boiling point.
Raw food should be stored separately from cooked or ready-to-eat food to avoid cross-contamination (contamination of one food through contact with another). Packaged food is preferable to loose products or those sliced to order, which should always be consumed promptly after purchase. The usual food hygiene rules, which apply to all foods and not only Listeria monocytogenes, should be scrupulously observed:
- Leftovers and pre-prepared food should be heated thoroughly before eating;
- Refrigerators should be cleaned regularly and disinfected with a bleach solution;
- Refrigerator temperatures should be monitored to ensure that they are low enough (4°C);
- Use-by dates should be observed;
- Hands and kitchen utensils should be washed after preparing raw food.
How many people are affected?
Vulnerable and immunocompromised people, pregnant women, infants, elderly people, people with cancer and transplant recipients are most at risk of developing severe forms of the disease.
The bacterium Listeria monocytogenes was first described in the 1920s, but listeriosis has only been considered a serious public health problem since 1981, when the foodborne origin of infection in humans was revealed during an outbreak in Canada. It has been a notifiable disease in France since 1998.
In mainland France, around 350 cases of listeriosis are reported each year. No large-scale outbreaks have been reported and the number of sporadic cases has fallen sharply in the past 15 years, especially in pregnant women and newborns. However, in recent years there has been an increase in cases of septicemia in elderly subjects, often those with comorbidities. In 2018, the most severe outbreak reported to date occurred in South Africa, with more than 1,000 infected patients, over 40% of whom were newborns. The source of contamination was identified as an industrially produced sausage that had been widely sold throughout the country.
March 2024