In December 2014, cases of HIV infection were detected in Roka, a village in Battambang province, northwestern Cambodia. Of more than 2,000 villagers tested for HIV, 242 people, aged from 2 to 89 years are diagnosed positive. Their common point: they were all treated by a "doctor" without a degree who reused the same syringes for several patients. Arrested in December 2014, he was sentenced at the end of 2015 to 25 years in prison.
How has iatrogenic transmission led to an unprecedented epidemic, resulting in an HIV prevalence of 11.8%, almost 20 times the national average? A team from the Institut Pasteur du Cambodge, in collaboration with local health authorities, traced the history of this epidemic. A "three-parameter" analysis was conducted, details Dr. Janin Nouhin, a researcher in the HIV / Hepatitis Unit: what is the profile of people infected with HIV, and is this virus associated with bloodborne viruses? Was this epidemic recent or had it lasted long before it was detected? What is the geographic extent of this epidemic and have other villages in Roka commune been affected?
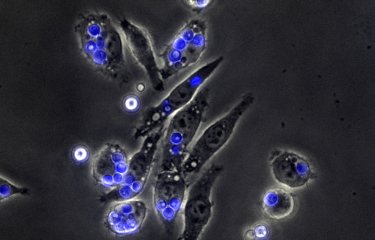
Numerous serological and molecular tests were conducted on 209 confirmed positive HIV cases, along with a field study with GPS mapping and interviews. The findings of these investigations revealed the existence of a massive, localized epidemic of HIV, associated with numerous co-infections with the hepatitis C virus (HCV): out of the 209 cases of HIV infection, 164 ( almost 8 out of 10) were co-infected with HCV. In contrast, less than 13% (27 patients) had co-infection with the hepatitis B virus (HBV). The use of a serological avidity test showed that about one-third of HIV cases were recent (<100 days). The same strategy, applied to HCV showed that almost 40% of acute hepatitis C, acquired less than 6 months ago.
Phylogenetic analyzes showed that 98% of the 209 patients were infected with the same virus (existence of a single monophyletic clade, genotype CRF01_AE). It can be assumed, according to the authors of the study, that a highly viremic Roka resident without antiretroviral drugs is the source of HIV contamination, via syringes reused by the fake doctor from 2013. HCV would have emerged earlier than HIV from at least three different sources of contamination.
Regarding HBV, two major reasons can be put forward for its lack of diffusion: even if a majority of Roka's inhabitants were not vaccinated, more than half were naturally protected against this virus (presence of anti-HBS antibodies), probably because of infections contracted in childhood. In addition, the proportion of inactive carriers (without viral replication) was high among HBV infected subjects.
Finally, the geographic study conducted in the field showed a positive correlation between HIV prevalence and a history of parenteral exposure with the pseudo-doctor. In particular, three geospatial hotspots of HIV were identified that correlated with high exposure to the practitioner.
"This unfortunate experience should serve as global warning," argues Janin Nouhin and the team from the Institut Pasteur du Cambodge, particularly in the Southeast Asia where many unnecessary injections are performed by people without medical training. In this context, it is necessary to limit risky injection practices and to promote oral medications. Since the discovery of this massive iatrogenic contamination, the patients in the commune of Roka are treated with antiretroviral drugs through the national health system.
Source: Rouet F, Nouhin J, Zheng DP, Roche B, Black A, Prak S, Leoz M, Gaudy-Graffin C, Ferradini L, Mom C, Mam S, Gautier C, Lesage G, Ken S, Phon K, Kerleguer A, Yang C, Killam W, Fujita M, Mean C, Fontenille D, Barin F, Plantier JC, Bedford T, Ramos A, Saphonn V. Massive Iatrogenic Outbreak of Human Immunodeficiency Virus Type 1 in Rural Cambodia, 2014-2015. Clin Infect Dis. 2017 Dec 4. doi:10.1093/cid/cix1071.