Symptoms can persist in some SARS-CoV-2 patients several months after infection. Scientists at the Institut Pasteur have demonstrated in an animal model that SARS-CoV-2 infects the brain and persists in the brainstem for up to 80 days after the acute infection phase. The presence of the virus is linked to symptoms of depression, impaired memory, and anxiety. Genes associated with neuronal metabolism and activity are deregulated in the brains of these animals, echoing similar processes observed in neurodegenerative diseases. This study was published in Nature Communications on July 22, 2025.
From the first wave of the COVID-19 pandemic, it was evident that certain symptoms persisted several weeks, and even months, after infection with the virus. This phenomenon, now known as "long COVID" (or post-COVID-19 syndrome), is characterized by a set of symptoms that generally appear within three months of initial infection and last at least two months. According to estimates from Santé publique France, long COVID affected 4% of the French adult population at the end of 2022. The most common chronic and debilitating symptoms of long COVID are: extreme fatigue, neurological complications ("brain fog"), respiratory difficulties (shortness of breath, tachycardia) and headaches.
Scientists from the Institut Pasteur's Lyssavirus, Epidemiology and Neuropathology Unit previously demonstrated that the olfactory epithelium may provide the virus with a gateway to the brain, potentially explaining certain neurological symptoms of long COVID. In this study, the scientists monitored the effects of SARS-CoV-2 infection on the central nervous system for up to 80 days after the acute infection phase in animal models.
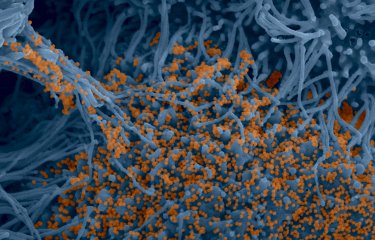
The scientists detected viral RNA of SARS-CoV-2 in most of the infected animals' nervous systems, most notably in the brainstem, for all investigated variants of SARS-CoV-2 (Wuhan, Delta, Omicron/BA.1) 80 days after the acute infection phase. Further analysis revealed viral replication activity in tissues, suggesting that the virus can continue to infect new cells even though the viral load is low. It therefore appears that the virus is able to persist at low levels in the brainstem.
The scientists subsequently investigated the impact of this viral RNA on brain metabolism. They observed that genes associated with neuronal metabolism and activity are deregulated in these animals' brains in a way that is reminiscent of the molecular signatures of neurodegenerative diseases, particularly Parkinson's, which involves deregulation of dopaminergic pathways.
"We observed that the expression of genes associated with dopamine metabolism is modified. SARS-CoV-2 infection appears to affect the production of dopamine, a neurotransmitter involved in regulating emotions and memory," explains Anthony Coleon, first author of the study and a PhD student in the Institut Pasteur's Lyssavirus, Epidemiology and Neuropathology Unit.
Furthermore, the scientists noted that the presence of the virus 80 days after the acute infection phase is linked to symptoms of depression, impaired memory, and anxiety. An assessment of these symptoms moreover revealed that these behavioral symptoms differed according to the animals' sex.
"Our study is the first to reveal the long-term biological impact of SARS-CoV-2 infection in animal models. It has revealed biological signatures that potentially explain some of the persistent symptoms observed in patients," adds Guilherme Dias de Melo, lead author of the study and scientist in the Institut Pasteur's Lyssavirus, Epidemiology and Neuropathology Unit.
"We are continuing our work to understand how infection induces a loss of dopamine neuron function. Our study has enabled us to identify a list of genes that are deregulated in the long term by SARS-CoV-2 infection. These genes provide potential targets for research on therapeutic molecules," he concludes.
Source
Hamsters with long COVID present distinct transcriptomic profiles associated with neurodegenerative processes in brainstem, Nature Communications, July 22, 2025
Anthony Coleon1, Florence Larrous1, Lauriane Kergoat1, Magali Tichit2, David Hardy2, Thomas Obadia3,4, Etienne Kornobis3,5, Hervé Bourhy1 and Guilherme Dias de Melo1*
1 Institut Pasteur, Université Paris Cité, Lyssavirus Epidemiology and Neuropathology Unit, F-75015 Paris, France
2 Institut Pasteur, Université Paris Cité, Histopathology Core Facility, F-75015 Paris, France
3 Institut Pasteur, Université Paris Cité, Bioinformatics and Biostatistics Hub, F-75015 Paris, France
4 Institut Pasteur, Université Paris Cité, G5 Infectious Diseases Epidemiology and Analytics, Paris, France.
5 Institut Pasteur, Université Paris Cité, Plate-forme Technologique Biomics, F-75015 Paris, France
*Corresponding author