For severely immunocompromised patients, a bone marrow transplant restores immune defenses and allows them to resume normal life. But after observing the nasopharyngeal mucosa, one of the body's first lines of immune defense, scientists from the Institut Pasteur, Université Paris Cité, Inserm and the Paris Public Hospital Network (AP-HP), in collaboration with the Imagine Institute, demonstrated a failure in certain immune mechanisms of some of these patients. The results of this study, published in the journal Blood on February 14, 2022, could pave the way for more effective treatment.
In patients with severe combined immunodeficiency (SCID),1 the immune system is compromised and unable to deal with the onslaught of microbial attacks from the environment. Alain Fischer, a founding member of the Imagine Institute at Necker-Enfants Malades Hospital (AP-HP), has followed these patients for the past 30 years and knows them well. "SCID patients need to be treated with an allogeneic bone marrow transplant,2 sometimes combined with pre-transplant chemotherapy to prevent graft rejection," explains the physician and immunologist. "This procedure cures patients and restores their immune system, but we had never previously taken a detailed look at what was happening in the nasal mucosa." The immune response machinery is highly complex and involves several components: agents in the innate immune response, which are particularly active in the mucosa of the gut, lungs and nose, and agents in the adaptive immune response, which circulate in the blood and lymph.
To help elucidate the way in which the innate immune system is regulated, James Di Santo, Head of the Innate Immunity Unit (Institut Pasteur/Inserm), proposed a study comparing the post-transplant immune systems of immunocompromised patients with the immune systems of healthy patients from the "Milieu Intérieur" cohort.3 "We already had nasopharyngeal samples taken with a simple nasal swab from some 1,000 subjects, and we were able to study the immune response using these samples," says the scientist. "The idea was to take the same type of samples from immunocompromised patients, together with a blood test, to see if there were any differences."
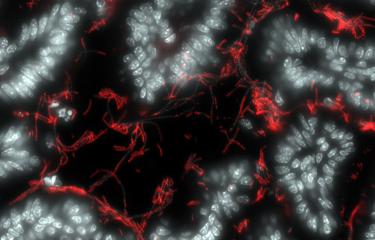
The scientists observed significant differences in some patients. Although in the healthy subjects and most of the immunocompromised patients the entire nasopharyngeal system had generally geared up to respond to attacks by forming a protective mucus layer, producing a large quantity of antibodies (especially IgA antibodies) and immune cells, and maintaining the microbiota, the nasal mucosa was disrupted in some transplant patients. In patients who were partially immunocompromised and had received only limited pre-transplant chemotherapy, the nasopharyngeal region had a smaller quantity of mucus, fewer IgA antibodies and cytokines4 and a prevalence of pathogenic bacteria. In other words, the mucosal immune system in these individuals was less active in dealing with daily attacks from pathogens. Their blood samples also revealed a selective deficiency in some circulating immune cells.
"We know that the immune cells in the blood produce cytokines, which stimulate the production of antibodies, and these antibodies in turn have the task of neutralizing pathogenic bacteria. If there is a deficiency in certain immune cells in the blood, it can trigger a chain reaction, ultimately leading to an imbalance in the microbiota known as dysbiosis," explains James Di Santo. For the first time, the scientists were able to observe innate immunity mechanisms in action in the nasal mucosa of these patients. This discovery could also prompt physicians to adjust their transplant protocol. "Patients who fail to recover their ability to produce IgA antibodies are potentially more vulnerable to respiratory infections," explains Alain Fischer. "We can compensate for this with an antibody replacement therapy, but the results of this new study also suggest that pre-transplant chemotherapy should be offered more systematically to ensure that their immune system is fully rebuilt."
(1) Not all types of severe combined immunodeficiency (SCID) have the same genetic origins or the same immunological profile. SCID is a very rare disorder, with the most common form only occurring in approximately 1 in 200,000 births each year.
(2) A transplant from one individual to another.
(3) Milieu Intérieur (LabEx): Lluis Quintana-Murci – Darragh Duffy – Milieu Intérieur [LabEx] – Research – Institut Pasteur
(4) Soluble messengers that mediate communication between cells in the immune system.
Source :
Defects in mucosal immunity and nasopharyngeal dysbiosis in HSC transplanted SCID patients with IL2RG/JAK3 deficiency, Blood, February 14, 2022
Pedro Goncalves1, Jean-Marc Doisne1, Toshiki Eri1, Bruno Charbit2, Vincent Bondet3, Celine Posseme3, Alba Llibre3, Milieu Intérieur Consortium†, Armanda Casrouge1, Christelle Lenoir4,5, Benedicte Neven4,5,6 Darragh Duffy3, Alain Fischer4,5,6,7 and James P. Di Santo1,*
1 Institut Pasteur, Université Paris Cité, Inserm U1223, Innate Immunity Unit, F-75015Paris, France
2 Institut Pasteur, Université Paris Cité, Center for Translational Science, F-75015 Paris, France
3 Institut Pasteur, Université Paris Cité, Translational Immunology Unit, F-75015 Paris, France
4 Inserm UMR 1163, F-75015 Paris, France.
5 Université de Paris Descartes Sorbonne Paris Cité, Imagine Institut, F-75015 Paris, France.
6 Department of Pediatric Immunology, Hematology and Rheumatology, Hôpital Necker-Enfants Malades, Assistance Publique-Hôpitaux de Paris (APHP), F-75015 Paris, France.
7 Collège de France, F-75231 Paris, France
doi : 10.1182/blood.2021014654