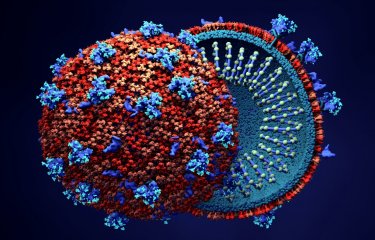
Innate immunity is the fastest-acting component of the immune system, but so far little is known about its role during infection with SARS-CoV-2. A few hours after an infection, the body emits an alarm signal, interferon, enabling cells that have not yet been infected to produce antiviral proteins. This phenomenon occurs well before the production of neutralizing antibodies. Scientists from the Institut Pasteur and the CNRS set out to investigate the consequences of SARS-CoV-2 infection for cell function and the antiviral role of innate immunity. Using real-time video microscopy, they showed that infected cells in culture can fuse with neighboring cells and die after forming giant cells known as "syncytia," composed of dozens of other cells. But interferon counters this phenomenon by inducing cellular proteins that prevent the fusion of infected cells.
These results showing the antiviral effect of innate immunity are available online on The EMBO Journal.
Little is yet known about the role of innate immunity in COVID-19. Various teams in different countries, including a French team, have recently demonstrated that severe forms are associated with a deficiency in interferon production.1 Interferon treatment has also shown beneficial effects in some patients. Interferon is a substance with antiviral activity that stimulates cells' natural defenses by inducing the synthesis of proteins that protect them from infection. Innate immunity occurs rapidly and can act in just a few hours, well before the other two forms of immunity – humoral immunity (the production of neutralizing antibodies that block virus entry into cells) and cell-mediated immunity (involving white blood cells such as cytotoxic lymphocytes that are capable of destroying infected cells).
Scientists from the Virus and Immunity Unit (Institut Pasteur/CNRS) investigated viral fusion, the mechanism by which viral membranes and cellular membranes fuse, allowing viral genetic material to enter the target cell. Viral fusion can also occur when the cell is infected and produces new viruses. Using real-time video microscopy, the scientists demonstrated that infected cells fuse with neighboring cells to form syncytia, or giant cells containing dozens of virus-producing cells, which eventually die. The role of syncytia in COVID-19 disease is not yet fully understood, but a team of Italian and British physicians recently demonstrated, by performing lung autopsies on patients who died of the disease, that syncytia was present in a high proportion of patients with severe forms.2
The authors of the study also examined how interferon affects syncytium formation. Interferon-induced transmembrane proteins (IFITMs) can play contradictory roles in different coronaviruses. The scientists demonstrated that in cells infected with SARS-CoV-2, IFITM proteins inhibit syncytium formation, thereby giving us an insight into the way in which interferon might control the evolution of COVID-19. These original observations, obtained in in vitro models with IFITM overexpression, now need to be reproduced in physiological models of human bronchial cells.
"Our findings give us a better understanding of the harmful effects of SARS-CoV-2 on cells and the role of innate immunity and interferon in controlling infection," comments Olivier Schwartz, lead author of the study and Head of the Virus and Immunity Unit at the Institut Pasteur.
2 https://www.medrxiv.org/content/10.1101/2020.06.22.20136358v1
Source
Syncytia formation by SARS-CoV-2 infected cell, The EMBO Journal, October 13, 2020
Julian Buchrieser1,2†, Jeremy Dufloo1,2†, Mathieu Hubert1,2†, Blandine Monel1,2†, Delphine Planas1,2,6†, Maaran Michael Rajah1,2, Cyril Planchais3, Françoise Porrot1,2, Florence Guivel-Benhassine1,2, Sylvie Van der Werf4,5, Nicoletta Casartelli1,2, Hugo Mouquet3, Timothée Bruel1,2, Olivier Schwartz1,2,6
1 Virus and Immunity Unit, Department of Virology, Institut Pasteur, Paris, France
2 CNRS-UMR3569, Paris, France.
3 Laboratory of Humoral Immunology, Department of Immunology, Institut Pasteur, INSERM U1222, Paris, France
4 Molecular Genetics of RNA Viruses, Department of Virology, Institut Pasteur CNRS UMR 3569; Université de Paris, Paris, France
5 National Reference Center for Respiratory Viruses, Institut Pasteur, Paris, France 6 Vaccine Research Institute, Créteil, France.
† first co-authors, (alphabetical order)