Age, biological sex, and human genetic factors influence the production of antibodies during the immune response. A team of scientists from the Institut Pasteur, the CNRS and the Collège de France have shown that these factors determine not only the quantity of antibodies produced but also the specific viral regions they target. This discovery could have major implications for the development of treatments that are better tailored to each individual's profile. The research was published in the journal Nature Immunology on February 16, 2026.
When the body is exposed to a virus, it defends itself by producing molecules called antibodies or immunoglobulins, which recognize pathogens and neutralize them. This is known as the humoral immune response, and it is essential in protecting us from infection. We know that genetic and non-genetic factors, such as age, biological sex, environment and lifestyle, influence how the immune system responds. Improving our understanding of the role of these factors is crucial for identifying individuals who are most vulnerable to infection and for developing more effective, personalized therapies. Research in this area has largely focused on one or a few viruses separately. As a result, little was known about how the humoral response to the full range of viruses infecting humans – the virome – varies from one person to another.
Scientists from the Institut Pasteur, the CNRS and the Collège de France have now shown that when attacked by the same virus, individuals produce antibodies that target different parts of that virus, and they identified the main factors underlying this variability.
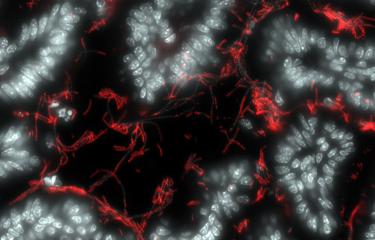
The scientists based their research on data from the Milieu Intérieur cohort, launched 15 years ago to study variations in the immune response in 1,000 healthy individuals. The project incorporates more than a hundred variables related to socio-economic status, lifestyle, medical history, and biological markers. Using an innovative sequencing technology, the scientists analyzed blood plasma samples to measure antibody responses against more than 90,000 fragments of viral proteins, covering a large number of viruses responsible for infections such as influenza, respiratory infections, gastroenteritis, and herpesvirus infections.

"A major strength of this study is its exhaustive quantification of the antibody repertoire. We were able to characterize exactly which parts of viral proteins are targeted by antibodies in each individual," explains Etienne Patin, CNRS Research Director in the Human Evolutionary Genetics laboratory at the Institut Pasteur and co-last author of the paper".
Etienne PatinCNRS Research Director in the Human Evolutionary Genetics laboratory at the Institut Pasteur and co-last author of the paper.
Age emerges as the dominant factor influencing antibody production – more than half of the antibody repertoire varies depending on age. Surprisingly, the scientists observed that for a given virus, some antibodies increase with age while others decrease, depending on the viral fragment targeted. This is the case for influenza H1N1 and H3N2: the antibodies in young adults mainly target a part of the viral surface protein known as hemagglutinin (HA), which evolves rapidly, whereas the antibodies in older individuals tend to target a more stable region of the same protein known as the stalk domain.
Biological sex also plays an important role. The humoral response to influenza A and B viruses differs between women and men, with women producing more antibodies against hemagglutinin (HA) while men tending to target other viral proteins (NP and M1), despite comparable vaccination rates between the two sexes.
Host genetic factors further shape antiviral immunity. The antibody repertoire is generated via a complex process of DNA rearrangement. "We identified mutations in genomic regions known to encode the immunoglobulin repertoire. These variants determine which genes are used to produce antibodies," continues Etienne Patin.
Finally, the scientists extended their study to include an African cohort, revealing population disparities in terms of the molecular targets of their antibody repertoires. For a given virus such as EBV (Epstein-Barr virus), antibodies can recognize different viral proteins depending on the geographical and epidemiological context. This difference can be explained by the level of exposure – Africans are more exposed to a particular strain of EBV in which the protein EBNA-4 is the primary antibody target.

"These results highlight the importance of extending our research to diverse populations worldwide, especially to populations that are under-represented in scientific research despite being among the most exposed to infectious diseases, such as those from tropical regions,"
Lluis Quintana-MurciHead of the Human Evolutionary Genetics laboratory at the Institut Pasteur, Professor at the Collège de France and co-last author of the paper.
"This study provides a detailed, integrated view of how age, sex and human genetics shape the antibody response," says Lluis Quintana-Murci. "It shows that these factors even determine which specific regions of a given virus are targeted by antibodies, with important implications for vaccine and therapeutic design."
"Our work goes well beyond conventional seroprevalence studies. The findings show that we need to consider inter-individual variation in antibody targets to develop a better understanding of the mechanisms that govern the human humoral response," concludes Etienne Patin.
See also
The team led by Simon Cauchemez at the Institut Pasteur has also recently described the diversity of antibodies directed against influenza virus H3N2. Through a population study in Nicaragua, the scientists showed that some antibodies directed against neuraminidase and the hemagglutinin stalk can not only protect against infection but also make the virus less contagious.
See the press release (December 22, 2025): Building a better vaccine: Study is first to ID expanded role of flu antibodies in preventing transmission
Source
Demographic and genetic factors shape the epitope specificity of the human antibody repertoire against viruses, Nature Immunology, 16 février 2026
Axel Olin1,2, Christian Pou3, Anthony Jaquaniello1,4, Jack Crook5, Ziyang Tan3, Maguelonne Roux1,6,14, Florian Dubois7,8, Bruno Charbit7,8, Dang Liu1, Françoise Donnadieu9, Laura Garcia9, Camille Lambert9, Emma Bloch9, Emmanuel Clave10, Itauá Leston Araujo10, Antoine Toubert10, Maxime Rotival1, Etienne Simon-Lorière5, Michael White9, Petter Brodin3,11, Darragh Duffy7,8, Lluis Quintana-Murci1,12,13,*, Etienne Patin1,13,*, on behalf of the Milieu Intérieur Consortium**
1 Human Evolutionary Genetics Unit, Institut Pasteur, Université Paris Cité, CNRS UMR2000, 75015 Paris, France
2 Division of Micro and Nanosystems, School of Electrical Engineering and Computer Science, KTH Royal Institute of Technology, 100 44 Stockholm, Sweden
3 Department of Women's and Children's Health, Karolinska Institutet, 17165 Solna, Sweden
4 Data Management Platform, Institut Pasteur, 75015 Paris, France
5 Evolutionary Genomics of RNA Viruses unit, Institut Pasteur, Université Paris Cité, CNRS UMR2000, 75015 Paris, France
6 Bioinformatics and Biostatistics Hub, Institut Pasteur, Université Paris Cité, 75015 Paris, France
7 Translational Immunology Unit, Institut Pasteur, Université Paris Cité, 75015 Paris, France
8 Single Cell Biomarkers UTechS, Institut Pasteur, Université Paris Cité, 75015 Paris, France
9 Infectious Disease Epidemiology and Analytics G5 Unit, Institut Pasteur, Université Paris Cité, INSERM U1347, 75015 Paris, France
10 Institut de Recherche Saint Louis, Université Paris Cité, INSERM UMR1342, 75010 Paris, France
11 Department of Immunology and Inflammation, Imperial College London, SW7 2AZ London, UK
12 Chair of Human Genomics and Evolution, Collège de France, 75005 Paris, France
13 These authors jointly supervised this work
14 Deceased