Simply comparing the total number of deaths across countries may provide a misleading representation of the underlying level of transmission of SARS-CoV-2, the virus that causes COVID-19, because of large differences in reported COVID-19 death rates in elderly populations in different countries.
The research conducted by the University of Cambridge, the Institut Pasteur and the CNRS, published today in the journal Nature, highlights the extent to which the very strong spread of Covid-19 in European nursing homes, along with incomplete death data for older age groups in some countries, make it difficult to use the total number of deaths to compare the level of circulation of the virus in different countries.
The researchers show that the number of Covid-19 deaths reported in those under 65 is probably a much more reliable indicator. These figures can give a clearer picture of the actual transmission of the virus and allow for more accurate comparisons between countries, which is crucial to guide government strategies to control the Covid-19 epidemic.
“Simply comparing the total number of deaths across countries can be misleading as a representation of the underlying level of transmission of SARS-CoV-2. Most deaths are in older people, but they are the least comparable across countries,” said Megan O’Driscoll, a PhD researcher in the University of Cambridge’s Department of Genetics and first author of the paper.
In countries including the UK, Canada and Sweden, the COVID-19 pandemic has disproportionately affected nursing home residents, who account for over 20% of all reported COVID-19 deaths. The level of SARS-CoV-2 transmission among the general population can be difficult to disentangle from these large outbreaks.
By contrast, some countries in Asia and South America have far fewer reported COVID-19 deaths in older people than expected. One potential explanation for these ‘missing deaths’ is that causes of deaths in elderly populations may be less likely to be investigated and reported as countries struggle to contain the epidemic.
“Nursing homes are enclosed communities of people, and once the virus gets in it can spread quickly resulting in higher levels of infection than in the general population. We’re seeing an excessively large number of deaths from COVID-19 in this older age group, particularly in countries that have many nursing homes,” said Dr Henrik Salje from the University of Cambridge’s Department of Genetics, co-lead author of the report.
He added: “It’s not just that residents are older than the general population, they are also generally more frail, so a 70-year old living in a nursing home is often more likely to die of COVID-19 than a 70-year old in the general population. To reduce the overall number of COVID-19 deaths it is vital to protect vulnerable elderly communities.”
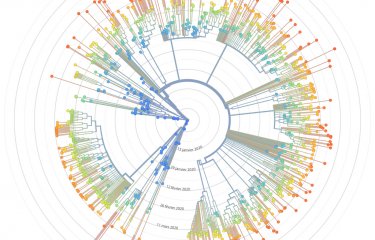
In their new model, the researchers integrated age-specific COVID-19 death data from 45 countries with 22 national-level seroprevalence surveys. These seroprevalence surveys estimate the number of people in a population with antibodies against the coronavirus. Antibodies indicate if a person has been infected with SARS-CoV-2 at some point, so are a good indicator of population-wide infection rates.
“By analysing the relative risk of death by Covid-19 according to age, we realised that many countries have the same age-specific mortality profile for people under 65. We were able to use this information to more reliably reconstruct the number of infections in different countries, even those for which no seroprevalence survey was carried out,” explained Simon Cauchemez, head of the Mathematical Modelling of Infectious Diseases unit[1] at the Institut Pasteur and co-lead author of the study.
The model can be used at a country-wide level to predict a person’s likelihood of dying from COVID-19 following infection, depending on their age. It can also be used to estimate a country’s total number of infections based on its number of COVID-19 deaths in different age groups, which is particularly useful in places where seroprevalence studies have not been conducted.
Using death data from under-65 age groups only, which is the most representative of transmission in the general population, the researchers estimate that by 1 September this year, an average of 5% of the population of the countries studied had been infected with SARS-CoV-2. However, in some places it was much higher, especially South America.
[1] Evolutionary genomics, modelling and health laboratory (GEMS, Institut Pasteur/CNRS)
Source
Age-specific mortality and immunity patterns of SARS-CoV-2 infection in 45 countries, Nature, November 2, 2020
Megan O’Driscoll1,2, Gabriel Ribeiro Dos Santos1,2, Lin Wang1,2, Derek A.T. Cummings3, Andrew S. Azman4,5, Juliette Paireau2,6, Arnaud Fontanet6,7, Simon Cauchemez2*, Henrik Salje1,2*
1. Department of Genetics, University of Cambridge, Cambridge, UK
2. Mathematical Modelling of Infectious Diseases Unit, Institut Pasteur, UMR2000, CNRS, Paris, France
3. Department of Biology and Emerging Pathogens Institute, University of Florida, Florida, USA
4. Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Baltimore, USA
5. Unit of Population Epidemiology, Division of Primary Care Medicine, Geneva University Hospitals, Geneva, Switzerland
6. Emerging Infectious Diseases Unit, Institut Pasteur, Paris, France
7. PACRI unit, Conservatoire National des Arts et Métiers, Paris, France
* : These authors contributed equally to this work.