Diagnosis of Plasmodium falciparum malaria using rapid diagnostic tests and treatment with artemisinin derivatives, the main component of the malaria treatments recommended by the World Health Organization (WHO), are under threat in the Horn of Africa. Scientists from the Laboratory of Parasitology and Medical Mycology at the University of Strasbourg and Strasbourg University Hospital, in collaboration with the Eritrean Ministry of Health, the Institut Pasteur, Columbia University in New York and WHO, have detected the emergence and spread in Eritrea of parasites with both artemisinin resistance and genome modifications that prevent their detection with rapid diagnostic tests, thereby jeopardizing malaria control and elimination campaigns in the region and potentially elsewhere in Africa. The research results were published on September 28, 2023 in the New England Journal of Medicine.
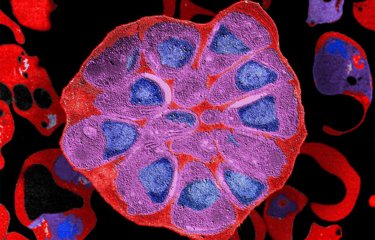
Malaria, a disease caused by parasites of the genus Plasmodium, represents a major public health problem worldwide. Plasmodium falciparum, responsible for severe forms, is found mainly in Sub-Saharan Africa, where a child dies of malaria every two minutes. In 2021, 247 million cases and 619,000 deaths were reported, a 6.4% increase compared with 2019.
Current strategies to fight malaria involve prevention, with the use of insecticide-treated bed nets; diagnosis, with the introduction of rapid diagnostic tests; and treatment, which must be effective. For more than 15 years, treatment for malaria episodes (which alternate between fever, shivering and chills, and severe sweating) caused by Plasmodium falciparum in Sub-Saharan Africa has been based on artemisinin-based combination therapies (ACTs). These highly effective treatments combine a potent, fast-acting artemisinin derivative and a partner drug with a long half-life that acts more slowly to eliminate residual parasites.
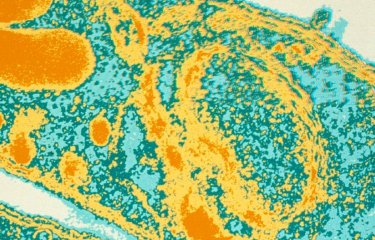
Unfortunately, in 2008, the first cases of artemisinin resistance were detected in South-East Asia. Resistance was defined by delayed parasite clearance from the bloodstream of patients treated with an ACT. In recent years, Plasmodium falciparum artemisinin resistance has also been reported in two regions of Sub-Saharan Africa, in Central Africa (Rwanda) and East Africa (Uganda).
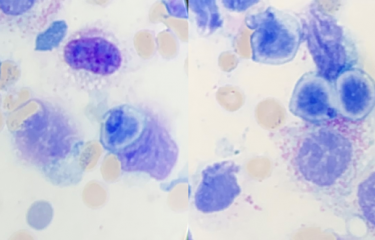
In this latest study, the scientists present the results of clinical trials conducted between 2016 and 2019 in Eritrea to assess the efficacy of two ACT treatments (artesunate/amodiaquine and artemether/lumefantrine) recommended for treating uncomplicated P. falciparum malaria. The clinical trials also aimed to estimate the proportion of patients with persistent P. falciparum parasitemia on day 3, the day after the last dose of ACT. In addition, the authors sought to identify molecular signatures in the Pfkelch13 gene associated with artemisinin resistance in parasites and to detect deletions of the hrp2 and hrp3 genes which are known to render rapid diagnostic tests ineffective in detecting parasites.
The data obtained revealed another hotspot of artemisinin resistance, in Eritrea. This novel area of resistance is more worrying than those observed in Rwanda and Uganda as the investigations reveal the emergence and spread of a new artemisinin-resistant variant, Pfkelch13 622I, accompanied by hrp2 and hrp3 gene deletions in around 17% of cases, making it impossible to detect these parasite strains using rapid tests. According to the published data, it seems that the phenomenon is not recent and that these strains have been circulating in western Eritrea for several years.
The findings therefore show how P. falciparum is capable of evading strategies introduced to control and eliminate malaria. "These data are a real cause for concern and undermine the quality of the health management of malaria patients in the region," warns Dr. Selam Mihreteab, a contributor to the study in Eritrea at the National Malaria Control Program, Ministry of Health. "We need to develop constant surveillance of the evolution of these parasites and their ability to spread," adds Dr. Lucien Platon, a PhD student at the Institut Pasteur (Malaria Parasite Biology and Vaccines Unit). "The strategies implemented in the Horn of Africa are under threat, not only because artemisinin resistant parasites are not detected by rapid tests but also because of the ability of malaria vectors to resist insecticides and because we have recently seen the arrival of a new mosquito species, Anopheles stephensi, capable of transmitting these strains in urban environments. There is a risk that these biological threats could lead to a rapid spread of these parasites in the region and beyond," analyzes Professor Didier Ménard, Director of the Institute of Parasitology and Tropical Diseases at the University of Strasbourg and a scientist in the Malaria Parasite Biology and Vaccines Unit at the Institut Pasteur.
Over the past two decades, the proactive strategy pursued by the Eritrean government has led to a significant reduction in malaria-related morbidity and mortality in the country. These new data seem to confirm that monitoring the emergence and spread of drug resistance must be a priority in areas such as Eritrea, where strategies to reduce malaria transmission are being effectively implemented, and that there is an urgent need to develop and introduce innovative control strategies.
This research received support from the Bill and Melinda Gates Foundation (WHO), the Global Fund (Ministry of Health in Eritrea), the Institut Pasteur, the French Government (National Research Agency), the University of Strasbourg (IdEX Program), and the United States Department of Defense and National Institutes of Health.
Source
Increasing Prevalence of Artemisinin-Resistant HRP2-Negative Malaria in Eritrea, New England Journal of Medicine, September 28, 2023
Selam Mihreteab*, B.Sc. Honores, Lucien Platon*, M.Sc., Araia Berhane, M.D., M.Sc., Barbara H. Stokes, Ph.D., Marian Warsame, M.D., Pascal Campagne, Ph.D., Alexis Criscuolo, Ph.D., Laurence Ma, B.S., Nathalie Petiot, B.S., Cécile Doderer-Lang, M.Sc., Eric Legrand, Ph.D., Kurt E. Ward, Ph.D., Assefash Zehaie Kassahun, M.D., M.Sc., Pascal Ringwald, M.D., Ph.D., David A. Fidock, Ph.D., Didier Ménard, Pharm.D., Ph.D.
* Dr. Selam Mihreteab and Lucien Platon contributed equally to this manuscript
National Malaria Control Program, Ministry of Health, Asmara, Eritrea (S.M.);
Institut Pasteur, Université Paris Cité, Malaria Genetic and Resistance Unit, INSERM U1201, F-75015 Paris, France (L.P., N.P., E.L., D.M.);
Institut Pasteur, Université Paris Cité, Malaria Parasite Biology and Vaccines, F-75015 Paris, (L.P., D.M.), Sorbonne Université, Collège doctoral ED 515 Complexité du Vivant, F-75015 Paris, France (L.P.);
Communicable Diseases Control Division, Ministry of Health, Asmara, Eritrea (A.B.);
Columbia University Irving Medical Center, Department of Microbiology & Immunology, New York, NY 10032, USA (B.H.S., K.W., D.A.F.);
Gothenburg University, School of Public Health and Social Medicine, Gothenburg, Sweden (M.W.);
Université de Strasbourg, Institute of Parasitology and Tropical Diseases, UR7292 Dynamics of Host-Pathogen Interactions, F-67000 Strasbourg, France (C.L-D., D.M.);
CHU Strasbourg, Laboratory of Parasitology and Medical Mycology, F-67000 Strasbourg, France (D.M.);
Institut Pasteur, Université Paris Cité, Bioinformatics and Biostatistics Hub, F-75015 Paris, France (P.C., A.C.);
World Health Organization office, Asmara, Eritrea (A. Z. K.); Institut Pasteur, Biomics Platform, C2RT, F-75015 Paris, France (L.M.);
Global Malaria Programme, World Health Organization, Geneva, Switzerland (P.R.);
Columbia University Irving Medical Center, Center for Malaria Therapeutics and Antimicrobial Resistance. Division of Infectious Diseases. Department of Medicine, New York, NY 10032, USA (D.A.F.).