Findings suggest future vaccines use natural antibodies to target both infection and spread.
Today’s influenza vaccines primarily prevent infection in individuals, but new research led by the University of Michigan and the Institut Pasteur suggests that incorporating antibodies generated after infection could lead to more powerful vaccines by also reducing person-to-person transmission.
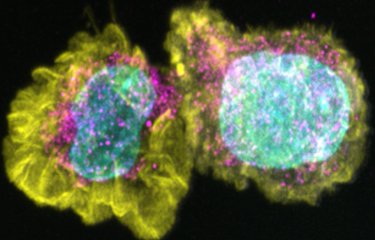
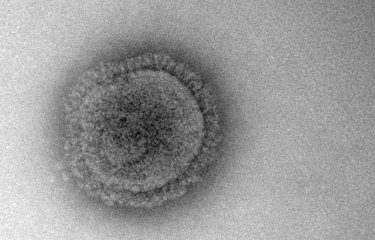
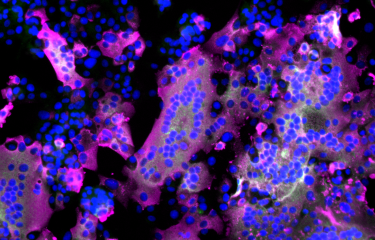
The influenza virus has two main surface proteins: one (called HA) allows the virus to attach to cells and infect them, the other (called NA) allows it to escape and spread. Current vaccines mainly target the HA protein. Researchers show that by also strengthening defenses against the NA protein, we would not only reduce infection in vaccinated individuals, but also reduce flu transmission from person to person.
"NA is a part of the influenza virus that has been relatively overlooked in vaccine design yet they play a key role not only in lowering infection risk but also in reducing how contagious someone becomes when infected," said Aubree Gordon, co-senior study author and director of the Michigan Center for Infectious Disease Threats and Pandemic Preparedness.
The study is published in the journal Nature Communications and was funded by the National Institutes of Health in the U.S. It comes amid warnings of a severe flu season ahead and as the first deaths of the 2025-2026 flu season are being recorded in the Northern Hemisphere. Influenza infects upwards of one billion people and leads to some 650,000 deaths globally each year. Lost productivity and hospitalizations due to the flu also result in major economic loss and burden.
"Modifying vaccines to include NA antibodies provides an extra layer of defense that's especially important for infants, immunocompromised individuals and others who can't mount strong vaccine responses," Gordon, an epidemiologist from the School of Public Health said. "This could also be very important if we were to have an influenza pandemic."
She helped lead a multinational research team that followed 171 Nicaraguan households and their 664 contacts over three influenza seasons - 2014, 2016, 2017. Almost all of the participants had never been vaccinated, allowing researchers to observe transmission patterns driven primarily by antibodies from infection.
Through bloodwork, virologic testing and the power of mathematical modeling, the researchers identified which antibodies were most effective at limiting spread.
Simon Cauchemez, epidemiologist and infectious disease modeller from Institut Pasteur and its Mathematical Modelling of Infectious Diseases Unit, is senior co-author with Gordon and said the detailed household data and modeling methods let the researchers chart and document how the antibodies reacted and which were most powerful in keeping an infected person from spreading the flu to people they came into contact with.
“Understanding which factors drive the spread of influenza is essential to design more effective control strategies but often challenging. Here, we were able to obtain such insight thanks to the analysis of very detailed data documenting influenza transmission in households with state-of-the-art modelling techniques," Cauchemez said.
"By studying immunity after infection,"the authors wrote, "we can identify which antibody responses are most protective and translate those insights into improved vaccine designs that provide stronger and longer-lasting protection."
Source
Anti-neuraminidase and anti-HA stalk antibodies reduce the susceptibility to and infectivity of influenza A/H3N2 virus, Nature Communications, December 11, 2025 (DOI : 10.1038/s41467-025-65283-0)
Gregory Hoy, University of Michigan Medical School et School of Public Health ; Thomas Cortier, Institut Pasteur et Sorbonne Université ; Hannah E. Maier et Abigail Shotwell, U-M School of Public Health ; Guillermina Kuan, Sustainable Sciences Institute et Centro de Salud Sócrates Flores Vivas, ministère de la Santé, tous deux à Managua (Nicaragua) ; Roger Lopez et Angel Balmaseda, Sustainable Sciences Institute, Managua (Nicaragua), et Laboratorio Nacional de Virología, Centro Nacional de Diagnóstico y Referencia, ministère de la Santé, Managua (Nicaragua) ; Nery Sanchez, Sergio Ojeda et Miguel Plazaola, Sustainable Sciences Institute, Managua (Nicaragua) ; Daniel Stadlbauer, Icahn School of Medicine ; Florian Krammer, Icahn School of Medicine, Center for Vaccine Research and Pandemic Preparedness, et Ignaz Semmelweis Institute.