Michaela Müller-Trutwin answers all our questions about the HIV virus and AIDS:
- What causes AIDS?
- What are the symptoms of the infection?
- How is HIV transmitted?
- How to get tested
- What are the treatments against HIV?
- How can I protect myself from infection?
What are the causes?
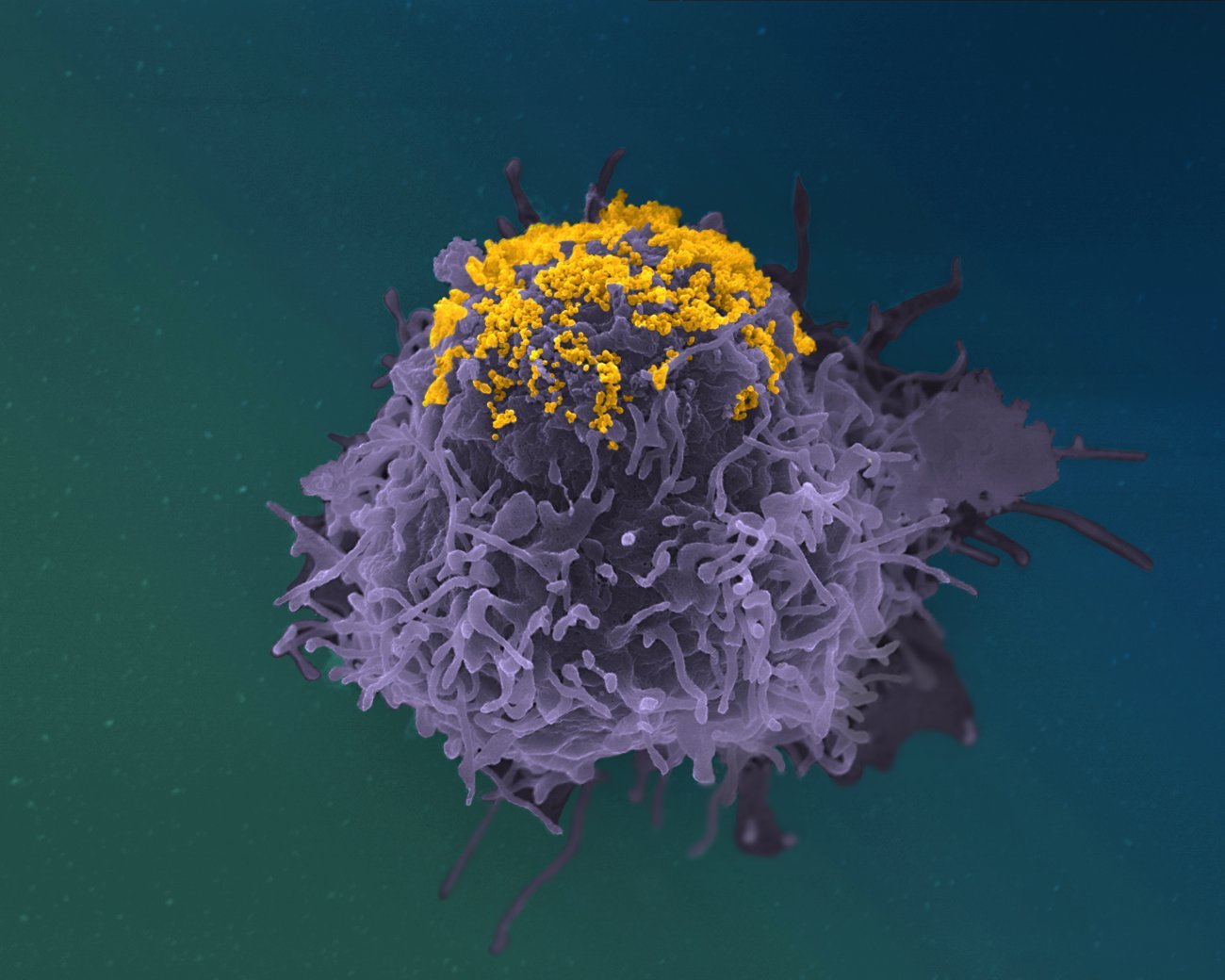
HIV targets and destroys T cells, white blood cells that play an essential role in the immune system.
For the first few years after infection, people with HIV generally have no clinical symptoms as their immune system continues to function normally.
In the absence of treatment, acquired immunodeficiency syndrome (AIDS) occurs around seven years after infection with HIV, when the immune system stops working because most of the body's T cells have been destroyed by the virus.
Over the long term, infected individuals can therefore develop what are known as "opportunistic" diseases, so called because they are caused by microorganisms that are usually harmless for people whose immune system is working normally. Opportunistic diseases include bacterial, fungal and parasitic infections, as well as some forms of cancer.
What are the symptoms?
The symptoms of HIV vary depending on the phase of infection. In the first weeks after infection, HIV-positive individuals may be asymptomatic or they may develop symptoms associated with the primary infection phase, characterized by clinical signs typical of flu such as high fever, muscle pain, headache and diarrhea.
Primary infection is followed by an asymptomatic phase that can last for several years. During this phase, the virus is present and infected individuals are contagious. HIV gradually weakens the immune system, leading to other symptoms such as weight loss, skin infections, cough, fever and diarrhea.
If left untreated, HIV progresses to AIDS, the final phase of infection.
How does HIV spread?
Human immunodeficiency virus (HIV) can spread through sexual contact or blood.
It can also spread from mother to child during pregnancy. This can occur:
- during the third trimester of pregnancy, when the virus can pass from mother to fetus via the placenta;
- at birth;
- when breastfeeding.
How is HIV infection diagnosed?
HIV is diagnosed by a blood test. People are generally tested for HIV following high-risk behavior (e.g. unprotected sex or needle sharing) or if they experience certain symptoms. The earlier HIV is diagnosed, the more effective the treatment.
What treatments are available?
There are currently no treatments that completely eliminate HIV from the body. The best treatments prevent HIV from multiplying, thereby keeping the immune system working properly. These treatments are referred to as highly-active antiretroviral therapy, or HAART, a regimen typically comprised of three viral replication inhibitors in a single pill.
First-generation antiretroviral drugs often caused side effects such as nausea, vomiting, fatigue, loss of appetite, fever, diarrhea and skin reactions.
For the vast majority of patients, new-generation drugs allow them to live a normal life if administered soon after infection. However, long-term side effects (such as weight gain and inflammation) cannot be ruled out. Research and clinical trials are being conducted with the aim of simplifying these therapies in people who respond to them effectively.
Taking antiretroviral medication during pregnancy reduces the risk of transmission to less than 1%, compared with 15 to 30% in the absence of treatment.
Patients are advised to start treatment as soon as possible after infection. This preserves the immune system as best as possible and also reduces the risk of passing HIV on. In these conditions, the life expectancy of HIV-positive individuals receiving treatment is close to that of the general population. Unfortunately, most cases of HIV are only detected after several years, and just 60% of people with HIV worldwide have access to treatment.
Rare individuals are able to resist infection
A tiny proportion of people living with HIV (less than 1%) are able to maintain the virus in their body at very low levels, often lower than the detection limit in the blood. This spontaneous control is often associated with a particular genetic background that gives rise to a very strong immune response specifically targeted at HIV.
A minority of patients (5 to 10%) who are monitored and treated in the first few weeks after infection become capable of controlling the virus. These people, known as post-treatment controllers, are considered to be in remission.
Some very rare individuals are even capable of resisting infection naturally. This ability comes from a mutation affecting a receptor situated at the surface of certain T cells which is normally used by HIV to infect them.
People at high risk of exposure but who remain HIV-negative have also been reported, but no explanation has been found.
How can HIV be prevented?
Prevention is primarily based on measures to stop HIV being passed on, such as the use of condoms or single-use needles.
There is currently no effective HIV vaccine.
Pre-exposure prophylaxis (PrEP) is reserved for specific people at risk of infection. PrEP involves taking a drug to prevent HIV infection. It is highly effective if taken as prescribed, reducing the risk of contracting HIV from sex by about 99% and from needle sharing by at least 74%.
Post-exposure antiretroviral therapy taken as prescribed after high-risk behavior reduces the virus to undetectable levels in the blood, considerably limiting the risk of transmission.
How many people are affected?
The World Health Organization (WHO) website regularly publishes updates with the latest figures on the HIV epidemic, including the number of HIV-positive individuals and the number of deaths.