Update - September 2025
What are the causes?
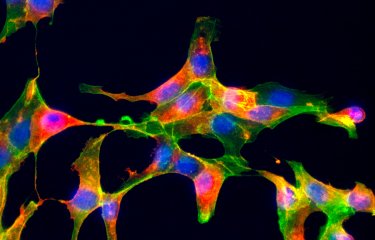
Chikungunya is a disease caused by the chikungunya virus, an RNA virus in the Alphavirus genus. Its mechanism of action is not well understood; it is thought that the virus mainly infects the muscles, joints, tissues containing white blood cells, and in some cases the central nervous system.
When an uninfected mosquito bites a person infected with the virus, the mosquito ingests it. The virus replicates and can be spread to humans when the mosquito bites again.
How does the disease spread?
The chikungunya virus is an arbovirus, meaning that it is transmitted by arthropods. Its vectors are female mosquitoes of the genus Aedes, which can be identified by their black and white stripes. The two species that spread the disease are Aedes albopictus and Aedes aegypti. The first is present in mainland France and second in the French West Indies, French Guiana, French Polynesia and New Caledonia. These two mosquitoes also transmit other arboviruses, including dengue, yellow fever and the Zika virus. The mosquitoes generally bite during the day, especially early in the morning and just before sunset.
What are the symptoms?
After an incubation period of 2 to 10 days, chikungunya virus infection causes joint pain, which is often very debilitating and mainly affects the wrists, fingers, ankles, feet and knees, and more rarely the hips and shoulders. The joint pain is often accompanied by headache together with fever, severe muscle pain, a skin rash on the torso and limbs, conjunctivitis, and the inflammation of one or more cervical lymph nodes. Bleeding gums and nosebleeds have also been reported.
In some cases, severe neurological manifestations can occur, including meningoencephalitis and peripheral neuropathy. These mainly affect elderly or immunocompromised people, as well as newborn infants who were infected in utero at the same time as their mother.
Chikungunya is rarely fatal; patients who die of the disease are likely to have had other health conditions. Most patients recover from the clinical symptoms fairly quickly, with fever and skin rashes clearing up in a few days. In some cases, the joint pain may last for weeks or even years, especially among older patients.
In the language of the Makonde people (an ethnic group from southern Africa), chikungunya means "to walk bent over," a reference to the posture adopted by patients because of the severe joint pain caused by the disease.
LEARN MORE
How is chikungunya diagnosed?
Chikungunya diagnosis is based on symptoms, travel patterns of patients in areas where the virus is endemic, and laboratory tests. Diagnostic tests include serological assays to detect antibodies for the virus and molecular biology tests such as PCR to detect the genetic material of the virus.
What treatments are available?
There are no specific antiviral treatments for chikungunya.
Medical treatment is purely symptomatic and is based on pain killers and anti-inflammatory drugs. Note that non-steroidal anti-inflammatory drugs should only be used if a diagnosis of dengue has been ruled out. These treatments cannot prevent chronic development of the disease. Corticosteroid treatment may be necessary for certain severe forms.
There is currently no vaccine for chikungunya but research is ongoing.
How can chikungunya be prevented?
Prevention of chikungunya infection is based on mosquito control measures. People should limit their exposure to mosquito bites by:
- wearing long clothes
- applying skin repellents
- using insecticides on clothes and mosquito nets
Larger-scale community-wide measures include using insecticides and removing stagnant water sources such as flower pots, used tires or bulky waste, which may become breeding grounds for mosquitoes.
In June 2024, the IXCHIQ vaccine received marketing authorization in Europe. It is already in use in the United States (see Chikungunya vaccines in the US).
In March 2025, in response to the chikungunya epidemic in La Réunion (French island in the Indian Ocean), the French National Authority for Health (HAS) recommended the use of this preventive vaccine for people at risk of severe forms of the disease who had never previously been diagnosed with infection by the virus. This included people aged 65 and over, as well as people aged 18 to 64 with comorbidities.
On April 26, 2025, following three serious events in Réunion involving people over 80 with comorbidities, linked to the IXCHIQ vaccine against chikungunya, the French health authorities decided to revise their vaccination recommendations. They removed people aged 65 and over, with or without comorbidities, from the vaccination target group. However, vaccination remains recommended for people aged 18 to 64 with comorbidities.
How many people are affected?
In 2023, the Aedes albopictus mosquito was present in 80% of départements in mainland France where the temperatures and humidity levels allow mosquito eggs to hatch. There are also large numbers of travelers returning from countries where the chikungunya virus is prevalent.
Between January and late July 2023, approximately 300,000 people were infected worldwide, leading to more than 300 deaths. The majority of cases were reported in Brazil and Paraguay.
Since it was first identified in Tanzania in 1952, chikungunya outbreaks have been reported in more than 60 countries across Africa, Asia, Europe and the Americas.
See the "Chikungunya in the United States" page - Centers for Disease Control and Prevention (CDC)
Further information about preventing and managing chikungunya can be found on the following sites:
- World Health Organization (WHO): Chikungunya (who.int)
- Santé publique France: Chikungunya – Santé publique France (santepubliquefrance.fr) (in French)

“The Geopolitics of the Mosquito” - Go further with our experts!