During the COVID-19 pandemic, the clinical spectrum observed among people infected with SARS-CoV-2 ranged from asymptomatic carriage to death. Researchers at the Institut Pasteur, the CNRS and the Collège de France, in collaboration with researchers around the world1 , have investigated the extent and drivers of differences in immune responses to SARS-CoV-2 across populations from Central Africa, Western Europe and East Asia. They show that latent cytomegalovirus infection and human genetic factors, driven by natural selection, contribute to population differences in immune response to SARS-CoV-2 and the severity of COVID-19. Understanding the factors underlying such population disparities could help to improve patient management in future epidemics. These results were published on August 9, 2023 in Nature.
The Institut Pasteur’s Human Evolutionary Genetics Unit2, led by Lluis Quintana-Murci, investigates how human populations differ in their immune responses to infection. These differences may result from different environmental exposures or from past population history, including natural selection, shaping the patterns of genetic diversity of human groups. In this study, published in Nature, the scientists investigated the extent and causes of disparities in the responses to the SARS-CoV-2 virus, focusing on populations from different geographic and ethnic backgrounds.
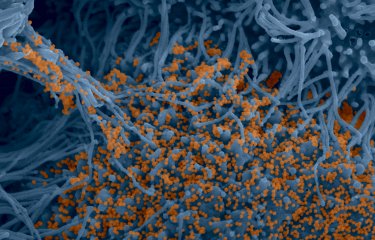
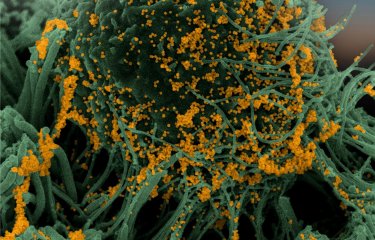
During the COVID-19 pandemic, the SARS-CoV-2 virus caused a wide range of clinical manifestation, from asymptomatic infection to fatal disease. Although advanced age remains a primary risk factor, male gender, comorbidities and various human genetic and immunological factors also contribute to disease severity. To study variations in immune responses to SARS-CoV-2 across human populations, scientists exposed immune blood cells from 222 healthy donors from Central Africa, Western Europe, and East Asia to the virus.
Single-cell RNA sequencing was used to analyze the SARS-CoV-2 responses of 22 blood cell types. These data were then combined with serological and genetic information collected from the same individuals, making it possible to assess the degree of disparity between populations in terms of their immune responses to SARS-CoV-2, and to identify contributing factors.
Scientists have identified around 900 genes that that respond differently to SARS-CoV-2 between populations. Using statistical genetic analyses, they show that these disparities are mainly due to variation in blood cellular composition: the proportion of each cell type differs from one population to another. We know that blood cell composition can be influenced by environmental factors such as exposure to cytomegalovirus (a human infection of the herpes family, which is usually harmless) and cytomegalovirus prevalence varies widely among populations: Central Africans present 99% seropositivity, in contrast to only 50% in East Asians and 32% in Europeans. The team found that an individual’s environment, specifically latent cytomegalovirus infection, will thus influence the immune cell response to SARS-CoV-2.
Furthermore, the scientists have identified around 1,200 human genes whose expression in response to SARS-CoV-2 is under the control of human genetic factors and the frequency of the alleles3 that regulate these genes can vary between the populations studied. Using population genetics approaches, they have identified recurrent selection events targeting genes involved in anti-viral functions. "We know that infectious agents have had a strong impact on human survival and exerted massive selective pressures that have shaped population genetic variation. We show that past natural selection has impacted present immune responses to SARS-CoV-2, particularly in people of East Asian ancestry, in whom coronaviruses generated strong selective pressures around 25,000 years ago," explains Maxime Rotival, a researcher in the Institut Pasteur's Human Evolutionary Genetics Unit and co-last author of the study.
Between 1.5% and 2% of the genomes of Europeans and Asians is of Neanderthal origin. There is growing evidence of links between Neanderthal ancestry and present-day immunity to infection. By comparing the 1,200 genes identified with the Neanderthal genome, the scientists have discovered dozens of genes that both alter antiviral mechanisms and result from ancient introgression between Neanderthals and modern humans (Homo sapiens). "Previous studies have shown the link between some of the genes identified in our study and the severity of COVID-19. Our comprehensive population-based study highlights the direct impact of genetic variants governing immune responses to SARS-CoV-2 on the severity of COVID-19. It also establishes links between past evolutionary events, such as natural selection or Neanderthal admixture, and current population disparities in immune responses and disease risk," explains Lluis Quintana-Murci, Head of the Human Evolutionary Genetics Unit at the Institut Pasteur, Professor at the Collège de France and co-last author of the study.
"By identifying the precise cellular and molecular pathways of the genetic variants associated with COVID-19 severity, this study paves the way for precision medicine strategies that could either identify high-risk individuals or facilitate the development of new treatments," adds Darragh Duffy, Head of the Institut Pasteur's Translational Immunology Unit.
This research was funded by the institutes mentioned above, and the French National Research Agency (ANR) (COVID-19-POPCELL, POPCELL-REG, COVIFERON), the European Horizon Health 2021 program (UNDINE), the French Foundation for Medical Research (FRM), the Allianz/Institut de France Foundation and the Fondation de France.
[1] Institut Imagine (France), Ghent University (Belgium), University of Rome (Italy), University of Detroit (USA), The Rockefeller University (USA), C2I Hong Kong (China), University of Melbourne (Australia).
[2] At the CNRS, this unit is known as the "Evolutionary Genomics, Modeling and Health Unit" (CNRS/Institut Pasteur).
[3] An allele is a version of a gene that is caused by a mutation. A gene has several alleles that perform the same function as the original gene, but in their own specific ways.
Source
Dissecting human population variation in single-cell responses to SARSCoV-2, Nature, 9 August 2023
Yann Aquino1,2,27, Aurelie Bisiaux1,27, Zhi Li1,27, Mary O'Neill1,27, Javier Mendoza-Revilla1, Sarah Helene Merkling3, Gaspard Kerner1, Milena Hasan4, Valentina Libri4, Vincent Bondet5,Nikaia Smith5, Camille de Cevins6,7, Mickael Menager6,7, Francesca Luca8,9,10, Roger Pique-Regi8,9, Giovanna Barba-Spaeth11, Stefano Pietropaoli11, Olivier Schwartz12, Geert Leroux-Roels13, Cheuk-Kwong Lee14, Kathy Leung15,16, Joseph T.K. Wu15,16, Malik Peiris17,18,19,Roberto Bruzzone18,19, Laurent Abel20,21,22, Jean-Laurent Casanova20,21,22,23,24, Sophie A.Valkenburg18,25, Darragh Duffy5,19, Etienne Patin1, Maxime Rotival1,28* & Lluis Quintana-Murci1,26,28*
1. Institut Pasteur, Universite Paris Cite, CNRS UMR2000, Human Evolutionary Genetics Unit, Paris, France.
2. Sorbonne Universite, College Doctoral, Paris, France.
3. Institut Pasteur, Universite Paris Cite, CNRS UMR2000, Insect-Virus Interactions Unit, Paris, France.
4. Institut Pasteur, Universite Paris Cite, Cytometry and Biomarkers UTechS, Paris, France.
5. Institut Pasteur, Universite Paris Cite, Translational Immunology Unit, Paris, France.
6. Universite Paris Cite, Imagine Institute, Laboratory of Inflammatory Responses and Transcriptomic Networks in Diseases, Atip-Avenir Team, INSERM UMR1163, Paris, France
7. Labtech Single-Cell@Imagine, Imagine Institute, INSERM UMR1163, Paris, France
8. Center for Molecular Medicine and Genetics, Wayne State University, Detroit, MI, USA.
9. Department of Obstetrics and Gynecology, Wayne State University, Detroit, MI, USA.
10. Department of Biology, University of Rome Tor Vergata, Rome, Italy
11. Institut Pasteur, Universite Paris Cite, CNRS UMR3569, Structural Virology Unit, Paris, France.
12. Institut Pasteur, Universite Paris Cite, CNRS UMR3569, Virus and Immunity Unit, Paris, France.
13. Ghent University and University Hospital, Ghent, Belgium.
14. Hong Kong Red Cross Blood Transfusion Service, Hospital Authority, Hong Kong SAR, China.
15. WHO Collaborating Centre for Infectious Disease Epidemiology and Control, School of Public Health, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China.
16. Laboratory of Data Discovery for Health (D24H), Hong Kong Science Park, Hong Kong SAR, China
17. Division of Public Health Laboratory Sciences, School of Public Health, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China.
18. HKU-Pasteur Research Pole, School of Public Health, The University of Hong Kong, Hong Kong SAR, China.
19. Centre for Immunology and Infection, Hong Kong Science Park, Hong Kong SAR, China
20. St. Giles Laboratory of Human Genetics of Infectious Diseases, The Rockefeller University, New York, NY, USA.
21. Laboratory of Human Genetics of Infectious Diseases, INSERM UMR1163, Necker Hospital for Sick Children, Paris, France.
22. Imagine Institute, Paris Cite University, Paris, France.
23. Department of Pediatrics, Necker Hospital for Sick Children, Paris, France.
24. Howard Hughes Medical Institute, New York, NY, USA.
25. Department of Microbiology and Immunology, Peter Doherty Institute for Infection and Immunity, University of Melbourne, Melbourne, Australia
26. Chair Human Genomics and Evolution, College de France, Paris, France.
27. These authors contributed equally.
28. These authors jointly supervised this work.
https://doi.org/10.1038/s41586-023-06422-9