What are the causes?
Malaria is transmitted to humans when they are bitten by an Anopheles mosquito which has been infected by a Plasmodium parasite after biting an infected person. The female mosquito injects the parasite into the body as she takes the blood meal she needs to lay her eggs. Male mosquitoes do not bite.
How is the parasite transmitted?
Plasmodium spreads between humans via mosquitoes, most often Anopheles gambiae on the African continent. Human-to-human contamination is possible from mother to child during pregnancy (transplacental transmission). Malaria can also be transmitted by blood transfusion.
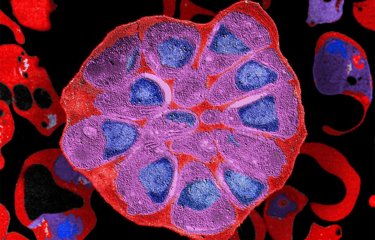
The Plasmodium life cycle is complex; it consists of two main stages – an asexual phase in humans and a sexual phase in mosquitoes.
First, the female mosquito bites a human and injects the parasite in the form of a sporozoite, which migrates via the bloodstream to the liver, where it replicates.
The parasites produced in the liver (merozoites) have a different form which enables them to infect red blood cells and continue replicating. They are ingested by another mosquito when it bites the human, and the cycle starts over again.
Between 2000 and 2019, four cases of post-transfusion malaria were reported in France.
The only way that malaria can be transmitted from one person to another is from a pregnant woman to her unborn child.
What are the symptoms?
The clinical signs of malaria are very varied. Fever develops 8 to 30 days after infection, sometimes with weakness, headache, muscle pain, vomiting, diarrhea and cough. Fever accompanied by shivers, cold sweats and heavy perspiration can occur cyclically because of the different phases in the parasite's life cycle. More severe symptoms may occur, such as difficulty breathing, bleeding, jaundice, extreme fatigue and convulsions.
In some cases, infected red blood cells can obstruct the blood vessels that irrigate the brain, which can be fatal.
In regions where malaria is highly endemic, some individuals are asymptomatic carriers of the parasite. After several years of chronic infection, some people tolerate the presence of the parasite and develop natural immunity.
How is infection diagnosed?
A blood test is needed for a confirmed laboratory diagnosis.
A malaria diagnosis is confirmed based on the identification of Plasmodium parasites (by microscopy or via a rapid diagnostic test).
Early diagnosis and treatment of malaria reduces disease, prevents deaths and contributes to reducing transmission.
What treatments are available?
Several antimalarial drugs can be used preventively on a short-term basis (for travelers to endemic regions) or administered in tablet form or by injection (the latter in hospital) to treat the disease.
The most common malaria drugs are:
- Artemisinin-based combination therapy medicines for P. falciparum malaria.
- Chloroquine for treatment of infection with the P. vivax parasite only in places where it is still sensitive to this drug.
- Primaquine can be added to the main treatment to prevent relapse of infection with P. vivax and P. ovale.
For several years now, parasites have been developing resistance to antimalarial drugs.
In 2008, for example, the first cases of artemisinin resistance were detected in South-East Asia. Resistance was defined by delayed parasite clearance from the bloodstream of patients treated with artemisinin-based combination therapy (ACT). In recent years, artemisinin resistance in Plasmodium falciparum has also been reported in two regions of Sub-Saharan Africa, in Central Africa (Rwanda) and East Africa (Uganda).
To find out more, see Malaria: treatment of Plasmodium falciparum malaria patients under threat in the Horn of Africa
How can malaria be prevented?
No means of prevention offers full protection. Even if appropriate treatment has been administered, a malaria attack may still occur, sometimes long after the disease was contracted. Any symptoms of fever, however mild, nausea, headache, aches or fatigue during or in the months following a stay in a tropical region must be considered as a potential case of malaria until proven otherwise, and emergency medical advice should be sought.
Prevention involves mosquito control measures such as mosquito nets and mosquito repellent. Preventive treatments may also be prescribed by a doctor before travel, depending on the destination (specifically the level of risk and the presence of resistance), the length of the trip and the person. Age, pregnancy, disease history, intolerance to antimalarial drugs or possible drug interactions are all factors to take into account when determining a suitable treatment. But no antimalarial drugs guarantee full protection against infection.
The only available malaria vaccine is RTS,S, but it is only moderately effective and only targets the parasite P. falciparum. Its use is recommended in addition to other measures to prevent severe forms of the disease.
Who is affected?
Malaria is present in around a hundred countries, mainly in impoverished tropical regions of Africa, Asia and Latin America. The African region is by far the most affected, with 94% of all reported cases of malaria. Outbreaks may occur with population movements to highly endemic areas. People traveling to these regions may also be affected.

“The Geopolitics of the Mosquito” - Go further with our experts!
September 2024