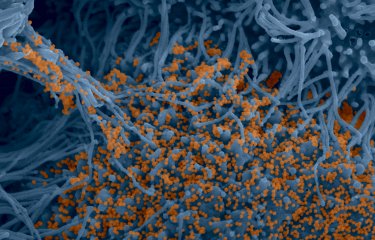
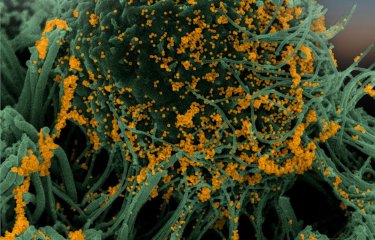
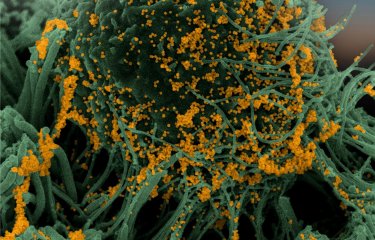
As part of the SEROCoV-HUS study, teams from Strasbourg University Hospital and the Institut Pasteur monitored 308 hospital staff who had previously contracted a mild form of SARS-CoV-2. The scientists demonstrated that neutralizing antibodies could be detected in 84% of them up to 6 months after infection, but that the level fell more quickly in men than in women. These results seem to suggest that immunity lasts longer in women than in men. The study was published as a preprint on the MedRxiv website. The results were then published on The Journal of Infectious Diseases on March 7th, 2021.
The evolution of the antibody response to SARS-CoV-2 in infected individuals remains poorly characterized. In an attempt to elucidate the evolution of the immune response, teams from Strasbourg University Hospital and the Institut Pasteur monitored 308 members of hospital staff who developed mild forms of COVID-19 that did not require hospital treatment.
The presence of SARS-CoV-2 antibodies was measured using three different techniques, two targeting the virus spike protein (S) and one targeting its nucleocapsid (N). The neutralizing activity of the various antibodies was also analyzed using a test that measures ability to block the virus.
The results revealed that men over the age of 50, or those with a body mass index (BMI) higher than 25, had higher antibody levels one month after the onset of symptoms compared with the rest of the individuals tested.
Between 3 and 6 months, anti-S antibodies and neutralizing antibodies persisted in 99% and 84% of individuals respectively, but anti-N antibodies were only found in 59% of individuals. This shows that depending on the test used, the seroprevalence of SARS-CoV-2 may be underestimated.
The scientists also showed that the levels of anti-S antibodies and neutralizing antibodies between 3 and 6 months fell more quickly in men than in women, independently of age and BMI. This result suggests that immunity to SARS-CoV-2 may last longer in women than in men.
Strasbourg University Hospitals and the Institut Pasteur are pursuing their work in this area so that they can play an active role in research on how the immune system responds to the virus and the efficacy of potential vaccination.
"We are studying the ability of the immune system to produce protective antibodies after SARS-CoV-2 infection and how long this immunity lasts. Our work in collaboration with the virologists and clinicians at Strasbourg Hospitals suggests that immunity may last longer in women than in men. These results need to be confirmed in a larger number of individuals. The next step will be to study the longer-term response of the immune system after infection and to compare it with the response obtained after vaccination, when vaccines become available," says Olivier Schwartz, Head of the Virus and Immunity Unit at the Institut Pasteur.
"Several studies have shown that COVID-19 manifests more severely in men than in women. This latest research conducted in collaboration with scientists from the Institut Pasteur suggests that this inequality continues after infection, with women retaining their protective antibodies for longer.
These new data, together with data about the reliability of serology tests over time, are very important for future evaluation of the vaccine response.
The next stage will be to study the other aspect of the immune response, the T-cell response, in the same cohort, to obtain a more comprehensive view of the immune response to SARS-CoV-2 and its evolution in mild forms of COVID-19," explains Professor Samira Fafi-Kremer, Director of the Institute of Virology in Strasbourg.
Source
Sex differences in the decline of neutralizing antibodies to SARS-CoV-2, The Journal of Infectious Diseases, March 7th, 2021
Ludivine Grzelak1,2,*, Aurélie Velay3,4,*, Yoann Madec5,*, Floriane Gallais3,4, Isabelle Staropoli1, Catherine Schmidt-Mutter6, Marie-Josée Wendling3,4, Nicolas Meyer7, Cyril Planchais8, David Rey9, Hugo Mouquet8, Ludovic Glady10, Yves Hansmann 11, Timothée Bruel1, Jérome De Sèze6,12, Arnaud Fontanet5, Maria Gonzalez 13, Olivier Schwartz1,14,&,# and Samira Fafi-Kremer3,4,&,#
1 Virus & Immunity Unit, Department of Virology, Institut Pasteur, CNRS UMR3569, Paris, France
2 Sorbonne Paris Cité, Université de Paris, Paris, France
3 CHU de Strasbourg, Laboratoire de virologie, F-67091 Strasbourg, France
4 Université de Strasbourg, INSERM, IRM UMR_S 1109, Strasbourg, France
5 Emerging Diseases Epidemiology Unit, Department of Global Health, Institut Pasteur, Paris, France
6 Centre d’investigation Clinique INSERM 1434, CHU Strasbourg, France
7 CHU de Strasbourg, Service de santé Publique, GMRC, F-67091 Strasbourg, France
8 Laboratory of Humoral Immunology, Department of Immunology, Institut Pasteur, INSERM U1222, Paris, France
9 CHU de Strasbourg, Pôle SMO, le Trait d’Union, F-67091 Strasbourg, France
10 CHU de Strasbourg, Laboratoire de Biochimie Clinique et Biologie Moléculaire, F-67091 Strasbourg, France.
11 CHU de Strasbourg, Service des infectieuses et tropicales, F-67091 Strasbourg, France
12 CHU de Strasbourg, Service de Neurologie, F-67091 Strasbourg, France
13 CHU de Strasbourg, Service de Pathologies Professionnelles, F-67091 Strasbourg, France
14 Vaccine Research Institute, Faculté de Médecine, INSERM U955, Université Paris-Est Créteil, Créteil, France
*co-first authors
&co-last authors
First publication online on November 19th, 2020