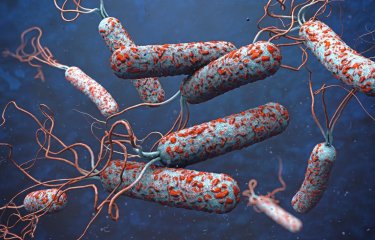
The seventh cholera pandemic has been affecting world regions since 1961. In successive waves, Vibrio cholerae bacteria have been accompanying humans in their travels and migrations, sometimes triggering devastating outbreaks, as is currently the case in Yemen. But what migratory pathways do these bacteria generally adopt? Can we monitor, or even anticipate, cholera outbreaks at global level? In an attempt to address these questions, scientists from the Institut Pasteur and the Wellcome Trust Sanger Institute, in collaboration with several international institutions, turned their attention to the cholera epidemic currently affecting Yemen. Using genomics tools, they were able to solve the mystery surrounding the history of the epidemic strain. Their research confirms that it is possible to gain a comprehensive overview of Vibrio cholerae circulation. The results were published in the journal Nature on January 2, 2019.
The arrival of the cholera[a] agent, Vibrio cholerae bacteria, on a new continent, stowed away in the gut of an infected traveler, does not systematically trigger a cholera outbreak. Sometimes the infection is not transmitted to other people, while on other occasions the bacteria spread rapidly throughout the population and wreak havoc, as is currently the case in Yemen. The war-torn country at the south-western tip of the Arabian Peninsula is experiencing the world's most severe cholera outbreak in recent years. Since September 2016, more than 1 million people have been affected by the acute diarrheal infection, which has claimed 2,300 lives. This prompted scientists from the Institut Pasteur and the Wellcome Trust Sanger Institute, in collaboration with several international institutions, to turn their attention to the Yemeni strain in a bid to shed light on its history.
"The cholera epidemic in Yemen initially raised several questions," explains Dr. François-Xavier Weill, Head of the Institut Pasteur's Enteric Bacterial Pathogens Unit. "The outbreak did not immediately spread as rapidly as may have been expected. There was a first, relatively minor wave in 2016, then a major resurgence in 2017. The two waves were so different that we wondered if they might actually have been caused by two separate bacterial strains," continues Marie-Laure Quilici, a scientist in the Institut Pasteur's Enteric Bacterial Pathogens Unit and Head of the National Reference Center for Vibrios and Cholera. To solve the enigma, the scientists decided to turn to genomics. In a previous study, this technique had already revealed that the cholera strains circulating in Africa for the last 40 years were recurrently imported from South Asia (1).
This time, the idea was to study bacterial isolates [b] that were collected – with the invaluable help of those working in the field, including members of the World Health Organization (WHO) and Médecins Sans Frontières –, in Yemen and neighboring countries as well as in South Asia between 2014 and 2017. "Using high-throughput sequencing techniques, we could see the accumulation of small, specific mutations known as single-nucleotide polymorphisms (SNPs) in the bacterial genome from one generation to the next, enabling us to trace the "family tree"," explained Dr. François-Xavier Weill. "And by crossing these genomic data with geographical and temporal data, we were able to monitor how the outbreaks spread, pinpoint links and shed light on how the outbreaks were interrelated."
After several months collecting and analyzing data, the results were revealed. The bacterial isolates collected during the two waves of cholera in Yemen belonged to the same strain. And this strain did not arrive directly from South Asia or the Middle East; but came from East Africa. Another surprising finding was that the Yemeni strain is sensitive not only to several antibiotics commonly prescribed to treat cholera, but also to polymyxins – resistance to which has been used as a marker of the seventh pandemics isolates since 1961. "It's very unusual to see a such massive epidemic with 1 million cases of cholera caused by an antibiotic-sensitive strain nowadays, because among bacteria, and V. cholerae in particular, we are generally observing an accumulation of antibiotic resistance determinants over time." explains Dr. François-Xavier Weill.
"This study once again illustrates how important it is to combine epidemiological data with laboratory data to monitor the circulation of strains and improve our efforts to control cholera. All countries need to be aware of this if they are to achieve the targets set by WHO's Global Task Force on Cholera Control,(2) namely reducing the cholera death toll by 90% by the year 2030," says Marie-Laure Quilici.
These new findings confirm the importance of genomic analysis in understanding the migration pathways used by cholera and establishing a comprehensive overview of the situation.
[a] an acute diarrheic disease caused by the ingestion of food or water contaminated by Vibrio cholerae bacteria. The disease spreads between humans in areas with inadequate access to clean water and sanitation.
[b] a bacterial colony isolated from the environment or from a patient sample.
(1) Genomic history of the seventh pandemic of cholera in Africa, Science, November 10, 2017
Source
Genomic insights into the 2016-2017 cholera epidemic in Yemen, Nature, January 2, 2019
François-Xavier Weill (1Y), Daryl Domman (2Y), Elisabeth Njamkepo (1), Abdullrahman A. Almesbahi (3), Mona Naji (3), Samar Saeed Nasher (3), Ankur Rakesh (4), Abdullah M. Assiri (5), Naresh Chand Sharma (6), Samuel Kariuki (7), Mohammad Reza Pourshafie (8), Jean Rauzier (1), Abdinasir Abubakar (9), Jane Y. Carter (10), Joseph F. Wamala (11), Caroline Seguin (12), Christiane Bouchier (13), Thérèse Malliavin (14), Bita Bakhshi (15), Hayder H. N. Abulmaali (16), Dhirendra Kumar (6), Samuel M. Njoroge (7), Mamunur Rahman Malik (9), John Kiiru (7), Francisco J. Luquero (4), Andrew S. Azman (17), Thandavarayan Ramamurthy (18), Nicholas R. Thomson (2,19), Marie-Laure Quilici (1)
Y : ont contribué équitablement.
- Institut Pasteur, Unité des Bactéries Pathogènes Entériques, Paris, 75015, France
- Wellcome Sanger Institute, Wellcome Genome Campus, Hinxton, CB10 1SA, UK
- National Centre of Public Health Laboratories (NCPHL), Sana'a, Yemen
- Epicentre, Paris, 75011, France
- Ministry of Health, Riyadh, 11176, Saudi Arabia
- Maharishi Valmiki Infectious Diseases Hospital, Delhi, 110009, India
- Centre for Microbiology Research, Kenya Medical Research Institute, P. O. Box 19464 – 00202, Nairobi, 00202, Kenya
- Pasteur Institute of Iran, Department of Bacteriology, Tehran, 13164, Iran
- WHO Regional Office for the Eastern Mediterranean (EMRO), Cairo, 11371, Egypt
- Amref Health Africa, P. O. Box 30125 – 00100, Nairobi, Kenya
- World Health Organization (WHO), Juba, 88 211, South Sudan
- Médecins Sans Frontières (MSF), P. O. Box 65650, Dubai, United Arab Emirates
- Institut Pasteur, Plate-forme Génomique (PF1), Paris, 75015, France
- Unité de Bioinformatique Structurale, UMR 3528, CNRS; C3BI, USR 3756; Institut Pasteur, Paris, 75015, France
- Department of Bacteriology, Faculty of Medical Sciences, Tarbiat Modares University, P. O. Box 14115-331, Tehran, Iran
- Central Public Health Laboratory (CPHL), Baghdad, Iraq
- Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Baltimore, 21231, MD, USA
- Translational Health Science and Technology Institute (THSTI), Faridabad, Haryana 121001, India
- London School of Hygiene and Tropical Medicine, London, WC1E 7HT, UK