What are the causes?
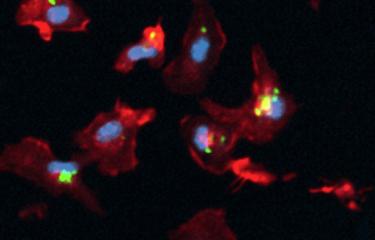
The active development of tuberculosis in people infected with Mycobacterium tuberculosis (also known as Koch's bacillus) depends on several factors, including genetic, immunological, nutritional and social aspects. It is thought that 5 to 10% of infected people will develop symptomatic tuberculosis during their lifetime. The bacillus can survive in a dormant state in the human body for years. Immunocompromised people are more likely to develop active tuberculosis. HIV and Koch's bacillus form a lethal combination, as HIV infection weakens the immune system, facilitating the spread of tuberculosis through the body. In the absence of treatment, tuberculosis is fatal in virtually all HIV-positive people.
How do the bacteria spread?
The infectious agent is spread through the air via bacteria-laden droplets produced when TB patients cough. Individuals can be infected by inhaling just a few of these contaminated droplets. A person with active but untreated tuberculosis can infect an average of 5 to 15 people a year. Poor sanitation and living conditions are often associated with the spread of tuberculosis.
What are the symptoms?
Most people with a latent tuberculosis infection do not develop symptoms and are not contagious. When an individual develops active tuberculosis, symptoms include a prolonged cough, fatigue, fever, night sweats, weight loss and chest pain.
Tuberculosis generally affects the lungs, but it can also impact the kidneys, spine, skin and brain.
Source: WHO
How is tuberculosis diagnosed?
Molecular assays are used for rapid diagnosis of tuberculosis. A skin test or blood test to detect infection can also be performed.
What treatments are available?
In the 1940s, there were no drugs available to treat tuberculosis. Today a combination of antibiotics is used to treat tuberculosis patients, but the treatment must be taken for at least six months (and up to two years in the event of multidrug-resistant strains). Incomplete or erratic treatment often leads to the emergence of antibiotic-resistant TB, which can then spread among the community. If treatable, these resistant TB cases are a hundred times more expensive to treat than TB cases that can be treated using conventional therapy.
The BCG (Bacillus Calmette-Guérin) is currently the only licensed tuberculosis vaccine. But the vaccine, which celebrated its 100th anniversary in 2021, is only partially effective. Even though it is very useful in preventing severe forms of disease in young children (nearly 90% efficacy in preventing tuberculous meningitis), it offers little protection against cases of pulmonary tuberculosis in adolescents and adults. It therefore cannot prevent transmission of the disease or eradicate the global epidemic.
How can tuberculosis be prevented?
Preventing tuberculosis involves screening and treating infected individuals to stop them developing the disease. BCG vaccination is used in several countries to prevent severe forms of tuberculosis in children. Infection control measures are crucial to prevent the disease from spreading, especially in healthcare facilities.
How many people are affected?
On average, 10 million people develop active tuberculosis each year. In 2022, 1.3 million people died of the disease, 167,000 of whom were also infected with HIV. More than 95% of tuberculosis deaths occur in developing countries, but tuberculosis remains a major public health problem in several industrialized countries, especially multidrug-resistant forms, which are difficult to treat and require lengthy therapy.
About one quarter of the world's population is currently infected with Mycobacterium tuberculosis. Just 30 countries account for 90% of all cases worldwide. The number of multidrug-resistant TB cases worldwide in 2019 was estimated to be 206,030, 10% more than in 2018.
In France, the average incidence is low; the most affected regions are French Guiana, Mayotte and Greater Paris (source: Santé publique France).

New weapons to fight bacteria
September 2024