What are the causes?
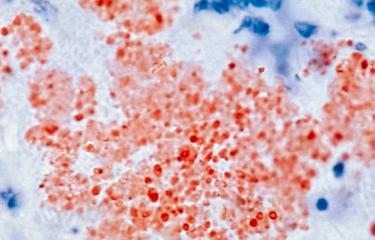
Plague is a disease caused by Yersinia pestis, a bacterium measuring approximately 1 to 3µm long. Yersinia pestis is extremely virulent. It was named after scientist Alexandre Yersin, who was the first to isolate the plague bacillus in 1894.
How does the disease spread?
Plague is mainly transmitted to humans by bites from fleas infected with Yersinia pestis, often carried by rodents such as rats.
The plague bacillus may also spread between humans via droplets of saliva expelled by an infected person when they cough. People infected in this way go on to develop pneumonic plague.
What are the symptoms?
In humans, there are two main forms of plague – bubonic, contracted via flea bite, and pneumonic, contracted via airborne transmission.
Bubonic plague, the most common clinical form, has an incubation period of a few days and is characterized by a very severe infectious syndrome, with high fever and deterioration of general health, accompanied by a swelling of the lymph node (bubo) draining the flea bite site. In 20 to 40% of cases, the bubo suppurates and the person recovers after a relatively long period of convalescence. Alternatively, the disease develops into septicemia and is quickly fatal. In some cases, the bacillus reaches the lungs. If appropriate early treatment is not administered, pneumonic plague is always fatal within three days.
How is plague diagnosed?
Clinical diagnosis of plague is based on patient symptoms and relevant history, such as travel to an endemic region or contact with a plague patient. This is followed by a laboratory analysis of fluid samples (blood, sputum or bubo samples) to confirm the presence of Yersinia pestis bacteria.
What treatments are available?
Early treatment is essential. Fluoroquinolones, tetracyclines and streptomycin are the antibiotics of choice for treating plague. These antibiotics are completely effective if administered early.
How can plague be prevented?
Early administration of tetracyclines, sulfonamides or fluoroquinolones is generally a highly effective preventive treatment strategy in close contacts of plague sufferers.
Travelers to endemic foci are advised to avoid contact with rodents and to protect themselves from flea bites with skin repellents effective in these endemic areas. In the event of contact with a plague patient with a cough, advice should be immediately sought from a doctor who can prescribe antibiotics as a preventive measure.
Prevention by vaccination was discontinued as the first vaccines caused side effects that were sometimes severe. Other vaccines were subsequently developed but they are not effective for pneumonic plague. Several vaccines are currently in the research stages but they are yet to be validated in humans.
How many people are affected?
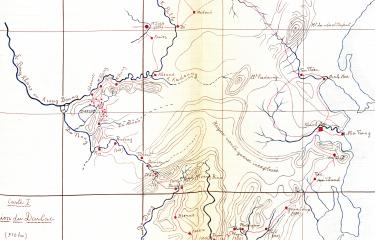
Nearly 50,000 human cases of plague were reported to the World Health Organization (WHO) by 26 countries in Africa, Asia and America between 1990 and 2020. Sub-Saharan Africa is currently the most affected region, with the Democratic Republic of the Congo, Uganda and above all Madagascar, which reports the highest number of human cases of plague in the world (between 250 and 500 cases a year). In Asia, the most active plague foci are in China. In 2020, cases were also reported in Mongolia. On the American continent, the main focus is Peru, but the United States is not exempt: indigenous cases of plague are reported on its west coast every year. No cases of plague have been reported in recent years in Oceania or Europe. The last cases in France occurred in Corsica in 1945.
One of the characteristics of plague outbreaks is their ability to "disappear" for a number of years and then suddenly resurface and cause a further outbreak. In India, an outbreak of pneumonic plague occurred in 1994, despite the fact that the disease was believed to have been eradicated nearly 30 years earlier. Around the same time, 128 cases of bubonic plague were reported in Mozambique following more than 15 years' absence; these cases spread to neighboring Zimbabwe and Malawi. An outbreak occurred almost simultaneously in Peru, with 1,031 cases in 1993-1994. Although closely spaced in time, there was probably no epidemiological link between the Asian, American and African outbreaks. In 1997, cases of plague in humans occurred in Jordan, following nearly 80 years' absence. Plague also reappeared in the Oran region of Algeria in 2003, following 50 years without an outbreak. An outbreak of pneumonic plague occurred in a diamond mine in the Democratic Republic of the Congo in December 2004, and a larger scale outbreak struck the same country in 2006.
Human cases of plague occurred in 2007 in Afghanistan, where no cases had ever previously been reported. More recently, plague re-emerged in Libya in 2009 after a gap of 25 years, and in Kyrgyzstan and Russia in 2013 after a gap of 30 and 34 years, respectively. Similarly, in 2016 a plague outbreak hit south-eastern Madagascar, a region outside the country's known plague endemic areas where no cases had been reported since 1950. In 2017, a major pneumonic plague outbreak in Madagascar affected a large number of regions, including the urban agglomerations of Antananarivo and Toamasina.
June 2024