What are the causes?
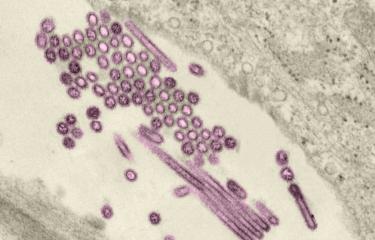
Influenza is an infectious disease caused by an enveloped RNA virus belonging to the Orthomyxoviridae family, which mainly affects the upper respiratory tracts (nose, throat and bronchi) and sometimes the lungs. Humans can be infected with three types of influenza virus: A, B and C.
- Type A viruses infect humans and various animal species, and the reservoir hosts are avian species (wild waterfowl, poultry) and various mammals (e.g. pigs). Type A viruses are classified into subtypes designated HxNy, based on their surface proteins hemagglutinin (H) and neuraminidase (N).
- Type B viruses almost exclusively infect humans. There are two type B virus lineages: B-Yamagata and B-Victoria.
- Type C viruses generally cause a very mild disease.
Type A and B viruses are responsible for seasonal outbreaks.
Type A viruses have pandemic (global epidemic) potential: like the influenza A(H1N1) pandemic of 2009/2010, which claimed 280,000 lives, which was the second pandemic in history caused by the H1N1 subtype; the first was the 1918 influenza pandemic (see below).
What are the symptoms?
The first symptoms appear 1 to 4 days after contamination. Infection generally lasts one week and is characterized by the sudden onset of fever, muscle and joint ache, headache, a general feeling of fatigue or weakness, and respiratory signs (dry cough, sore throat and runny nose).
Most infected individuals recover within a week with symptomatic treatment (antipyretics, hydration, cough medicine and rest).
Some vulnerable individuals are at risk of developing severe influenza that may lead to hospitalization in intensive care, respiratory support or even death, for example people over the age of 65, pregnant women, the morbidly obese (body mass index, or BMI, >40 kg/m2), diabetics, immunodeficient patients, people with chronic conditions (cardiovascular diseases, respiratory diseases), and infants.
Please note that influenza should not be confused with influenza-like illness
- Influenza is the infection caused by an influenza virus, which has the same symptoms as influenza-like illness.
- Influenza-like illness is a range of symptoms (fever, respiratory signs, aches, headache, etc.) caused by a respiratory virus that may be different from influenza, for instance respiratory syncytial virus (RSV), rhinovirus, parainfluenza virus or adenovirus.
- If necessary, doctors may take a respiratory sample for laboratory testing during an influenza-like illness to establish whether or not it is influenza.
How does the infection spread?
Influenza viruses are easily spread by aerosol transmission via microdroplets ejected when infected individuals cough, sneeze or speak. They can also be spread by hand, when people touch a contaminated surface and then bring their hands close to their nose, which is why barrier measures are so important during outbreaks (see below).
Influenza viruses enter the body through airborne transmission via the nose or throat. They replicate in the respiratory epithelium, where new viral particles are produced. Viral replication is localized and leads to necrosis of the ciliated respiratory epithelium which is accompanied by excessive bronchial mucus secretion.
Cold temperatures aid influenza virus survival which partly explains why outbreaks occur in winter in temperate climates.
How is infection diagnosed?
Biological testing of nasal swab specimens is performed.
What treatments are available?
Treatment is symptomatic and good hygiene habits limit the spread. A specific antiviral treatment may also be prescribed.
The antivirals available in France are influenza neuraminidase* inhibitors such as oseltamivir (Tamiflu®), which is effective against type A and B viruses and can be taken orally. It reduces disease duration and symptom severity if taken early, i.e. within 48 hours following the onset of symptoms. It can also reduce the risk of complications and death.
Another neuraminidase inhibitor, zanamivir (Relenza®) can be administered intravenously in hospital in the event of resistance to oseltamivir.
There are also adamantanes which are protein inhibitors, but the viruses have often been reported as resistant to this drug.
These antivirals are prescribed as curative medicine, and oseltamivir can also be given as a preventive measure in some situations (an outbreak in a nursing home for example).
*Neuraminidase: viral surface glycoprotein with enzyme activity that enables newly-formed viral particles to be released and spread in the mucus.
How can the disease be prevented?
- In the event of an outbreak, personal protective measures are needed to avoid becoming infected or infecting others, i.e. wearing a mask, using disposable tissues, coughing and sneezing into your arm or sleeve, washing your hands regularly and airing your home. If you are ill, avoid contact with vulnerable individuals.
- In addition to hygiene measures, the annual influenza vaccine is the most effective means of protection and it reduces severe forms of influenza. It is strongly recommended for the most vulnerable individuals (see above), but also for medical staff, people in nursing homes and for all other people in direct contact with vulnerable individuals. The vaccine is effective for 6 to 9 months.
Influenza viruses are constantly undergoing genetic changes, so the composition of the influenza vaccine has to be changed every year to incorporate the most recent circulating strains. The vaccine's efficacy depends above all on the age and immune status of the vaccinated individual, as well as the similarity between the selected vaccine strains and circulating influenza viruses.
How many people have been affected?
"Spanish flu," the most severe pandemic in modern history, was responsible for 20 to 50 million deaths worldwide between 1918 and 1919. Other pandemics followed in 1957, 1968... and more recently in 2009.
Influenza outbreaks vary according to the season. They occur in temperate regions between November and April in the northern hemisphere, and between April and October in the southern hemisphere. It is also impossible to predict how strong or severe an outbreak will be. In France, seasonal influenza affects 2 to 6 million people and claims approximately 10,000 lives each year.
Find out more: Burden and impact of seasonal influenza: assessment of the last 10 epidemics | Santé publique France (santepubliquefrance.fr) (in French)
Pandemics are rare but the 20th century witnessed three:
- the most severe, the 1918 pandemic, or "Spanish flu,", caused by the H1N1 subtype, spread across the world and was responsible for 20 to 50 million deaths between 1918 and 1919;
- the Asian flu of 1957, caused by the H2N2 subtype;
- and the 1968 "Hong Kong" flu, caused by the H3N2 subtype.
In 2009, the year of the last influenza pandemic, the virus responsible was a new variant of the H1N1 subtype, resulting from genetic exchanges (called reassortments) between a human virus, an avian virus and two swine viruses.
November 2023