An international effort including researchers from University of California San Francisco (UCSF), Gladstone Institutes, Icahn School of Medicine at Mount Sinai and Institut Pasteur (Paris) unveils promising compounds for clinical testing against COVID-19. The study, led by UCSF Quantitative Biosciences Institute Director, Nevan Krogan, PhD, reveals that some drugs may fight COVID-19 while another promotes infectivity. These results were published in Nature, on April 30 at 3:00 p.m.
An international team of more than 120 scientists has detailed the impact of 75 over-the-counter prescription and development-stage drug compounds on SARS-CoV-2, the virus that causes COVID-19. Several of these agents show promise in blocking SARS-CoV-2 replication in laboratory experiments. One compound investigated in the research, a common ingredient in over-the-counter cough medicines, appears to have the potential to promote the growth of the virus.
The collaborative study, published in Nature on April 30, 2020, was assembled and led by Nevan Krogan, PhD, director of the Quantitative Biosciences Institute at UC San Francisco and a senior investigator at Gladstone Institutes. As the first hints of the pandemic emerged in January, over a matter of just a few weeks, Krogan formed a rapid-response research team of dozens of scientists and clinicians -- hailing from UCSF, Gladstone, Icahn School of Medicine at Mount Sinai in New York, and Institut Pasteur in Paris -- to search for potential treatments for COVID-19.
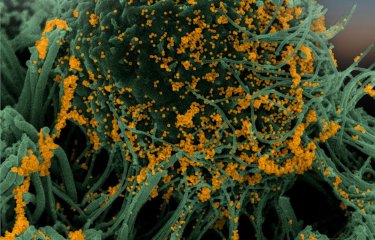
Rather than focusing on an antiviral approach to block SARS-CoV-2, the researchers first combined biological and computational techniques to create a “blueprint” of more than 300 human proteins that the virus requires to infect human cells and to thrive and replicate in the body. They then explored the question of which drugs, both those that are currently marketed as well as those in development, might be repurposed to treat SARS-CoV-2 infection by targeting those human proteins.
The researchers emphasized that while the drugs identified in the study are promising, they have only been tested against the virus in laboratory experiments. The researchers do not advocate anyone prescribing and/or using the drugs unless human clinical trials find them to be safe and effective.
Repurposed Compounds that Show Promise for Fighting COVID-19; Further Research Needed
Looking at a list of drugs that interact with the protein blueprint, UCSF researchers Brian Shoichet, PhD, and Kevan Shokat, PhD, led studies employing chemical biology and computational approaches. Two drug categories emerged as promising agents to effectively reduce viral infectivity: protein translation inhibitors (including zotatifin and ternatin-4/plitidepsin), and drugs that modulate proteins inside the cell known as Sigma1 and Sigma2 receptors, including progesterone, PB28, PD-144418, hydroxychloroquine; the antipsychotic drugs haloperidol and cloperazine; siramesine, an antidepressant and anti-anxiety drug; and the antihistamines clemastine and cloperastine.
Among the protein translation inhibitors, the strongest antiviral effect in vitro was seen with zotatifin, which is currently in clinical trials for cancer, and ternatin-4/plitidepsin, which is FDA-approved for the treatment of multiple myeloma.
Among the Sigma1 and Sigma2 modulators, the antipsychotic haloperidol, used to treat schizophrenia, showed antiviral activity against SARS-CoV-2. Olanzapine, used to treat both schizophrenia and bipolar disorder, had no measurable effect on the virus. Two potent antihistamines, clemastine and cloperastine, displayed antiviral activity, as did PB28 and to a lesser extent the female hormone progesterone.
“While a large amount of COVID-19 therapeutic development research focuses on the antivirals and vaccines, we’ve taken a different approach, targeting the human counterparts and vulnerabilities required for viral infection in a human cell,” said Krogan. “Our work leverages approved and development-stage molecules and will help to focus clinical trials toward the most promising agents to combat COVID-19. We also continue to search for additional agents that target the human proteins used by SARS-CoV-2 to expand the armamentarium against the virus,” he said.
“While these are early data, we have a high degree of confidence in the results, since similar observations on the antiviral activity of these drugs arose from work done independently at both Mount Sinai and Institut Pasteur. Research at this speed and magnitude could only have been accomplished through a collaborative effort from several scientists at multiple institutions, each bringing unique but complementary skill sets towards a common research goal,” said Adolfo García-Sastre, PhD, Professor in the Department of Microbiology and Director of the Global Health and Emerging Pathogens Institute of Icahn School of Medicine at Mount Sinai in New York. García-Sastre led the virological studies along with Marco Vignuzzi, PhD, principal investigator in the Viral Populations Unit at Institut Pasteur in Paris.
Vignuzzi commented, “This study provides novel potential antiviral strategies that need to be explored, and it is unique in that it extends our knowledge on our basic understanding of how the virus interacts with the host.”
PB28 Shows Significantly Greater Antiviral Activity than Hydroxychloroquine
Among drugs targeting Sigma1 and Sigma2 receptors, a preclinical compound called PB28 had approximately 20 times greater antiviral activity than hydroxychloroquine in laboratory experiments, which is being studied as a potential therapy for COVID-19 in multiple clinical trials.
Theory for Cardiac Side Effects of Hydroxychloroquine
The new study presents a possible explanation for the serious cardiac side effects observed in some halted clinical studies of hydroxychloroquine. The researchers showed that, in addition to targeting the Sigma1 and -2 receptors, hydroxychloroquine also binds to a protein known as hERG, which is critical for regulating electrical activity in the heart. These laboratory findings may help explain the possible risks associated with this agent as a potential therapy for COVID-19.
Caution Urged for Dextromethorphan
Finally, the cough suppressant dextromethorphan, which acts on Sigma1 receptors, promoted viral infection in the laboratory experiments, and the researchers said that its use merits caution and warrants further study in the context of COVID-19.
Next Step: Testing Compounds in Animal and Human Clinical Studies for COVID-19
Krogan said the next step is to further investigate the most promising compounds to advance them as quickly as possible through clinical trials. “We are working with several pharma and biotech companies to evaluate the antiviral effectiveness and safety of drug candidates that showed the most promise in our laboratory experiments,” he said. “Conversely, because our research shows that dextromethorphan promotes SARS-CoV-2 infection in the laboratory, we urge that this compound be used prudently during the pandemic.”
Shokat added, “Our collaborative efforts have successfully mapped the proteins in the human body associated with SARS-CoV-2 infection, which has informed swift, science-based drug discovery. Uncovering the proteins targeted by this coronavirus has unveiled compounds across different drug classes that might have otherwise not have been obvious to study in a viral setting.”
Background on innovative scientific approach
The researchers introduced the coronavirus proteins into human cells in culture. Once inside the cells, the viral proteins found specific human proteins that they could latch onto—very much as they would during a normal infection.
After identifying these proteins and determining small molecules known to bind them based on prior scientific research, the scientists identified 69 molecules that seemed most promising based on their targeting specificity.
Subsequently, the team assessed the impact of 47 of these compounds in cells infected with live virus, as well as an additional 28 compounds known to act on two key targets identified by other methods. These experiments were required to quickly establish robust and quantitative viral replication inhibition assays under high biocontainment to study the impact of these compounds on the biological cycle of the SARS-CoV-2
Aside from helping scientists quickly identify the most promising drug candidates to pursue, which may result in the initiation of new clinical trials, these results also provide broad insights into SARS-CoV-2 infection. Scientists can use this information to understand or anticipate the effect of experimental treatments already attempted in the clinic. Additionally, this novel approach for drug discovery can be leveraged across other viral and non-viral diseases.
Source
A SARS-CoV-2 protein interaction map reveals targets for drug repurposing, Nature, April 30, 2020
David E. Gordon1,2,3,4,35, Gwendolyn M. Jang1,2,3,4,35, Mehdi Bouhaddou1,2,3,4,35, Jiewei Xu1,2,3,4,35, Kirsten Obernier1,2,3,4,35, Kris M. White5,6,35, Matthew J. O’Meara7,35, Veronica V. Rezelj8,35, Jeffrey Z. Guo1,2,3,4, Danielle L. Swaney1,2,3,4, Tia A. Tummino1,2,9, Ruth Huettenhain1,2,3,4, Robyn M. Kaake1,2,3,4, Alicia L. Richards1,2,3,4, Beril Tutuncuoglu1,2,3,4, Helene Foussard1,2,3,4, Jyoti Batra1,2,3,4, Kelsey Haas1,2,3,4, Maya Modak1,2,3,4, Minkyu Kim1,2,3,4, Paige Haas1,2,3,4, Benjamin J. Polacco1,2,3,4, Hannes Braberg1,2,3,4, Jacqueline M. Fabius1,2,3,4, Manon Eckhardt1,2,3,4, Margaret Soucheray1,2,3,4, Melanie J. Bennett1,2,3,4, Merve Cakir1,2,3,4, Michael J. McGregor1,2,3,4, Qiongyu Li1,2,3,4, Bjoern Meyer8, Ferdinand Roesch8, Thomas Vallet8, Alice Mac Kain8, Lisa Miorin5,6, Elena Moreno5,6, Zun Zar Chi Naing1,2,3,4, Yuan Zhou1,2,3,4, Shiming Peng1,2,9, Ying Shi1,2,4,11, Ziyang Zhang1,2,4,11, Wenqi Shen1,2,4,11, Ilsa T. Kirby1,2,4,11, James E. Melnyk1,2,4,11, John S. Chorba1,2,4,11, Kevin Lou1,2,4,11, Shizhong A. Dai1,2,4,11, Inigo Barrio-Hernandez12, Danish Memon12, Claudia Hernandez-Armenta12, Jiankun Lyu1,2,9, Christopher J. P. Mathy1,2,13,14, Tina Perica1,2,13, Kala B. Pilla1,2,13, Sai J. Ganesan1,2,13, Daniel J. Saltzberg1,2,13, Ramachandran Rakesh1,2,13, Xi Liu1,2,9, Sara B. Rosenthal15, Lorenzo Calviello1,16, Srivats Venkataramanan1,16, Jose Liboy-Lugo1,16, Yizhu Lin1,16, Xi-Ping Huang17, YongFeng Liu17, Stephanie A. Wankowicz1,2,11,18, Markus Bohn1,2,9, Maliheh Safari1,2,19, Fatima S. Ugur1,2,4,9, Cassandra Koh8, Nastaran Sadat Savar8, Quang Dinh Tran8, Djoshkun Shengjuler8, Sabrina J Fletcher8, Michael C. O’Neal20, Yiming Cai20, Jason C. J. Chang20, David J. Broadhurst20, Saker Klippsten20, Phillip P. Sharp4, Nicole A. Wenzell1,2,4, Duygu Kuzuoglu1,2,4,21,22, Hao-Yuan Wang1,2,4, Raphael Trenker1,2,23, Janet M. Young24, Devin A. Cavero3,26, Joseph Hiatt3,25,26, Theodore L. Roth3,25,26, Ujjwal Rathore3,26, Advait Subramanian1,2,26, Julia Noack1,2,26, Mathieu Hubert10, Robert M. Stroud1,2,19, Alan D. Frankel1,2,19, Oren S. Rosenberg1,2,19,27, Kliment A Verba1,2,9, David A. Agard1,2,19, Melanie Ott1,2,3,27, Michael Emerman28, Natalia Jura1,2,4,23, Mark von Zastrow1,2,4,29, Eric Verdin1,27,30, Alan Ashworth1,2,21, Olivier Schwartz10, Christophe d’Enfert31, Shaeri Mukherjee1,2,26, Matt Jacobson1,2,9, Harmit S. Malik24, Danica G. Fujimori1,2,4,9, Trey Ideker1,32, Charles S. Craik1,2,9,21, Stephen N. Floor1,16,21, James S. Fraser1,2,13, John D. Gross1,2,9, Andrej Sali1,2,9,13, Bryan L. Roth17, Davide Ruggero1,2,4,21,22, Jack Taunton1,2,4, Tanja Kortemme1,2,13,14, Pedro Beltrao1,12, Marco Vignuzzi8, Adolfo García-Sastre5,6,33,34, Kevan M. Shokat1,2,4,11, Brian K. Shoichet1,2,9 & Nevan J. Krogan1,2,3,4,5
1 QBI COVID-19 Research Group (QCRG), San Francisco, CA, 94158, USA.
2 Quantitative Biosciences Institute (QBI), University of California San Francisco, San Francisco, CA, 94158, USA.
3 J. David Gladstone Institutes, San Francisco, CA, 94158, USA.
4 Department of Cellular and Molecular Pharmacology, University of California San Francisco, San Francisco, CA, 94158, USA.
5 Department of Microbiology, Icahn School of Medicine at Mount Sinai, New York, NY, 10029, USA.
6 Global Health and Emerging Pathogens Institute, Icahn School of Medicine at Mount Sinai, New York, NY, 10029, USA.
7 Department of Computational Medicine and Bioinformatics, University of Michigan, Ann Arbor, MI, 48109, USA.
8 Viral Populations and Pathogenesis Unit, CNRS UMR 3569, Institut Pasteur, 75724, Paris, cedex 15, France
9 Department of Pharmaceutical Chemistry, University of California, San Francisco, CA, 94158, USA.
10 Virus and Immunity Unit, Institut Pasteur, 75724, Paris, cedex 15, France.
11 Howard Hughes Medical Institute, San Francisco, CA, USA.
12 European Molecular Biology Laboratory (EMBL), European Bioinformatics Institute, Wellcome Genome Campus, Hinxton, Cambridge, UK.
13 Department of Bioengineering and Therapeutic Sciences, University of California, San Francisco, CA, 94158, USA.
14 The UC Berkeley-UCSF Graduate Program in Bioengineering, University of California San Francisco, San Francisco, CA, USA.
15 Center for Computational Biology and Bioinformatics, Department of Medicine, University of California San Diego, San Diego, CA, 92093, USA.
16 Department of Cell and Tissue Biology, University of California, San Francisco, CA, 94143, USA.
17 Department of Pharmacology, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, North Carolina, 27599-7365, USA.
18 Biophysics Graduate Program, University of California, San Francisco, CA, USA.
19 Department of Biochemistry and Biophysics, University of California San Francisco, San Francisco, CA, 94158, USA.
20 Zoic Labs, Culver City, CA, 90232, USA.
21 Helen Diller Family Comprehensive Cancer Center, University of California, San Francisco, CA, 94158, USA.
22 Department of Urology, University of California, San Francisco, San Francisco, CA, 94143, USA.
23 Cardiovascular Research Institute, University of California San Francisco, San Francisco, CA, 94158, USA.
24 Division of Basic Sciences, Fred Hutchinson Cancer Research Center, Seattle, WA, 98109, USA.
25 Medical Scientist Training Program, University of California, San Francisco, CA, 94143, USA.
26 George William Hooper Foundation, Department of Microbiology and Immunology, University of California San Francisco, San Francisco, CA, 94143, USA.
27 Department of Medicine, University of California San Francisco, San Francisco, CA, USA.
28 Division of Human Biology, Fred Hutchinson Cancer Research Center, Seattle, WA, 98103, USA.
29 Department of Psychiatry, University of California San Francisco, San Francisco, CA, 94158, USA.
30 Buck Institute for Research on Aging, Novato, CA, 94945, USA.
31 Direction Scientifique, Institut Pasteur, 75724, Paris, cedex 15, France.
32 Division of Genetics, Department of Medicine, University of California San Diego, San Diego, CA, 92093, USA.
33 Department of Medicine, Division of Infectious Diseases, Icahn School of Medicine at Mount Sinai, New York, NY, 10029, USA.
34 The Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai, New York, NY, 10029, USA.