One to two weeks after contracting COVID, the SARS-CoV-2 virus generally becomes undetectable in the upper respiratory tract. But does that mean that it is no longer present in the body? To find out, a team from the Institut Pasteur specialized in HIV, in collaboration with a French public research institute, the Alternative Energies and Atomic Energy Commission (CEA), conducted a study on lung cells in an animal model. The results show not only that SARS-CoV-2 is found in the lungs of certain individuals for up to 18 months after infection, but also that its persistence appears to be linked to a failure of innate immunity (the first line of defense against pathogens). This research was published in the journal Nature Immunology on November 2, 2023.
Some viruses persist in the body in a discreet and undetectable manner after causing an infection. They remain in what are known as ‘viral reservoirs’. This is the case for HIV, which remains latent in certain immune cells and can reactivate at any time. It could also be the case for the SARS-CoV-2 virus which causes COVID-19. At least, that is the hypothesis put forward by a team of scientists from the Institut Pasteur in 2021, and which has now been confirmed in a preclinical model of a non-human primate. "We observed that inflammation persisted for long periods in primates that had been infected by SARS-CoV-2. We therefore suspected that it could be due to the presence of the virus in the body," explains Michaela Müller-Trutwin, Head of the Institut Pasteur's HIV, Inflammation and Persistence Unit.
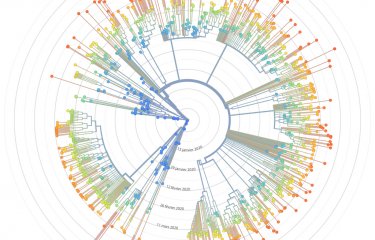
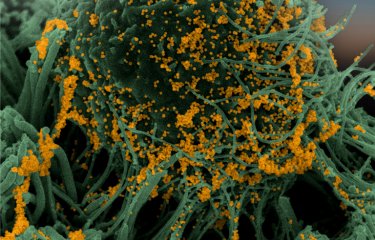
To study the persistence of the SARS-CoV-2 virus, scientists at the Institut Pasteur, in collaboration with the CEA’s IDMIT (Infectious Disease Models for Innovative Therapies) center, analyzed biological samples from animal models that had been infected by the virus. Initial results from the study indicate that viruses were found in the lungs of some individuals 6 to 18 months after infection, even though the virus was undetectable in the upper respiratory tract or blood. Another finding was that the amount of persistent virus in the lungs was lower for the Omicron strain than for the original SARS-CoV-2 strain. "We were really surprised to find viruses in certain immune cells – alveolar macrophages – after such a long period and when regular PCR tests were negative," points out Nicolas Huot, first author of the study and researcher in the Institut Pasteur's HIV, Inflammation and Persistence Unit. "What's more, we cultured these viruses and were able to observe, using the tools we developed to study HIV, that they were still capable of replicating."
To understand the role of innate immunity in controlling these viral reservoirs, the scientists then turned their attention to NK (natural killer) cells. "The cellular response of innate immunity, which is the body's first line of defense, has been little studied in SARS-CoV-2 infections until now," says Michaela Müller-Trutwin. "Yet it has long been known that NK cells play an important role in controlling viral infections." The study shows that in some animals, macrophages infected with SARS-CoV-2 become resistant to destruction by NK cells, while in others, NK cells are able to adapt to infection (known as adaptive NK cells) and destroy resistant cells, in this case macrophages.
The study has therefore shed light on a mechanism that may explain the presence of ‘viral reservoirs’: while individuals with little or no long-term virus had adaptive NK cell production, individuals with higher levels of virus had not only an absence of adaptive NK cells, but also a reduction in NK cell activity. Innate immunity therefore appears to play a role in the control of persistent SARS-CoV-2 viruses. "We will be embarking on a study of a cohort infected with SARS-CoV-2 at the start of the pandemic to find out whether the viral reservoirs and mechanisms identified are related to cases of long COVID. But the results here already represent an important step in understanding the nature of viral reservoirs and the mechanisms that regulate viral persistence," says Michaela Müller-Trutwin.
This research was funded primarily by a family of major donors as part of the COVID Research Program call for projects.
Source
SARS-CoV-2 viral persistence in lung alveolar macrophages is controlled by IFN-γ and NK cells, Nature Immunology, November 2, 2023
Nicolas Huot1, Cyril Planchais2, Pierre Rosenbaum2, Vanessa Contreras3, Beatrice Jacquelin1, Caroline Petitdemange1, Marie Lazzerini1, Emma Beaumont1, Aurelio Orta-Resendiz1, Félix A. Rey4, R. Keith Reeves5,6,7,8, Roger Le Grand3, Hugo Mouquet2 & Michaela Müller-Trutwin1
1Institut Pasteur, Université Paris-Cité, HIV, Inflammation and Persistence Unit, Paris, France.
2Institut Pasteur, Université Paris Cité, INSERM U1222, Humoral Immunology Unit, Paris, France.
3Université Paris-Saclay, INSERM, CEA, Immunologie des Maladies Virales, Auto-Immunes, Hématologiques et Bactériennes (IMVA-HB/IDMIT/UMR1184), Fontenay-aux-Roses & Kremlin Bicêtre, France.
4Institut Pasteur, Université Paris-Cité, Structural Virology Unit, CNRS UMR3569, Paris, France.
5Center for Virology and Vaccine Research, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA.
6Division of Innate and Comparative Immunology, Center for Human Systems Immunology, Department of Surgery, Duke University School of Medicine, Durham, NC, USA.
7Ragon Institute of Massachusetts General Hospital, MIT, Cambridge, MA, USA.
8Duke Research and Discovery at RTP, Duke University Health System, Durham, NC, USA.