“The Geopolitics of the Mosquito” - Go further with our experts!

After investigating cotton, water and paper, the Institut Pasteur’s ambassador, Erik Orsenna, has turned his attention to mosquitoes in his new book, Géopolitique du moustique (The Geopolitics of the Mosquito). In this report we look more closely at the efforts of the Institut Pasteur scientists to understand mosquitoes and the diseases they transmit, which are known as vector-borne diseases. We also take the opportunity to feature a few extracts from our ambassador’s book.
“When they buzz around our ears at night, they're not merely disturbing us – they’re telling a story: they're giving us their take on globalization. It's a story on a planetary scale of frontiers annihilated, constant mutation and struggles for survival. Ultimately it is the story of a ménage à trois: the mosquito, the parasite and its prey (in other words us vertebrates)", says Erik Orsenna in his book, Géopolitique du moustique, Petit précis de mondialisation IV (The Geopolitics of the Mosquito: a Brief Summary of Globalization IV), published by Fayard, which will be available in bookshops from April 3, 2017.
In order to write this book, Erik Orsenna tracked mosquitos and traveled through a number of countries where mosquito-borne diseases are rife. He also made regular visits to the Institut Pasteur in Paris. It was during one of these visits that this ambassador for the Institut Pasteur met Anna-Bella Failloux, who heads the Arboviruses and Insect Vectors Unit, and François Rodhain, an eminent medical entomologist who is now an honorary professor of the Institut Pasteur. He also visited Africa, America and Asia, where he met Amadou Alpha Sall at the Institut Pasteur in Dakar, Senegal, Mirdad Kazandji, at the Institut Pasteur in French Guiana (Cayenne), Didier Fontenille at the Institut Pasteur in Cambodia (Phnom Penh), and scientist colleagues including Gilles Bœuf, professor at Pierre and Marie Curie University, and Frédéric Simard from MIVEGEC (Infectious Diseases and Vectors: Ecology, Genetics, Evolution and Control), who is a former student of Didier Fontenille. "Very few people are as fascinating to listen to," said Erik Orsenna. They helped him achieve an understanding of mosquitoes. What are mosquitoes? Where do they live? How can we get rid of them? In this report, the Institut Pasteur experts offer a deeper insight into mosquitoes, in particular those belonging to the Aedes family, which are vectors of dangerous viruses.

Over a hundred mosquito-borne diseases
Many of the communicable diseases that cause a quarter of all deaths globally are vector-borne diseases (in other words carried by a vector). This vector is in the form of a hematophagous arthropod (insect or tick), which transmits the pathogen from one vertebrate host to another (human or other). Mosquitoes are the most common vectors. "There are over one hundred mosquito-borne diseases, including dengue, which affects over 50 million people each year, and chikungunya. These are arboviruses, in other words viruses that are transmitted between vertebrates via a bite from a hematophagous vector," explained Anna-Bella Failloux.
Vector-borne diseases cause nearly one million deaths annually. The most serious of these is malaria, which threatens over half the world's population but which is rife mainly in Sub-Saharan Africa. Dengue is present on most continents. This is without taking into account vector-borne diseases that are more localized geographically, such as Chagas disease, leishmaniasis, sleeping sickness, Lyme disease, etc.
the re-emergence of a disease
The incidence of dengue is currently rising rapidly, and it is now considered to be a "re-emerging" disease. WHO estimates that 50 million people are infected annually, 500,000 of whom contract dengue hemorrhagic fever, which is fatal in over 20% of cases.
Dengue is also known as "tropical flu", and is a viral disease transmitted to humans via Aedes mosquitoes. There are four viral strains – DEN-1, DEN-2, DEN-3 and DEN-4, which are all very different from each other.
"Classical" dengue starts with a high fever, headaches, nausea, vomiting, joint and muscle pain and a skin rash similar to that of measles. These symptoms are followed by conjunctival hemorrhaging, nose bleeds or ecchymosis. Although highly debilitating, it is not considered serious. Hemorrhagic dengue, on the other hand, which develops in about 1% of dengue cases, is extremely serious. In addition to a high fever, patients suffer from multiple hemorrhages in the gastrointestinal tract, skin and brain. Children under 15, in particular, may die from hypovolemic shock (a rapid decrease in blood volume). It is not known precisely why some people go on to develop the hemorrhagic form of the disease. However, infection by one of the strains provides lifelong protection from that particular strain, but not from the three others. It would appear that successive infections increase the risk of developing hemorrhagic dengue.
On an epidemiological level, three and a half billion people live in high-risk areas. Although initially present in tropical and subtropical regions, dengue has now spread to Europe, where the first two indigenous cases were reported in 2010. In 2014 the mosquito vector was present in 18 French departments. There is a very real risk of propagation if infected individuals enter mainland France.
Discover the Defeat Dengue program at the Institut Pasteur.
At the Institut Pasteur
Dengue is a much-studied disease at the Institut Pasteur. Several teams are working on multidisciplinary, complementary topics in both fundamental and applied research.
These teams* are brought together in an interdisciplinary working group, whose strategy is to target the various different aspects of the outbreak in an effort to bring it under control. They are aiming at jointly developing innovative therapeutic tools: a new vaccine candidate, prognostic markers, and a strategy for controlling vectors of the virus.
*Teams led by Anavaj Sakuntabhai, Frédéric Tangy, Anna-Bella Failloux, Valérie Caro and Hugues Bédouelle.
3,546 species of mosquito on Earth

Did you know that the Earth is home to no fewer than 3,546 species of mosquito? Only about one hundred of these sting humans. Of these, two species are notable for their capacity to carry arboviruses, which are responsible for diseases such as yellow fever, dengue, chikungunya and Zika virus disease that kill about 60,000 people annually. These are Aedes mosquitoes – Aedes albopictus (or tiger mosquito - in French) and its alter ego, Aedes aegypti. Aedes mosquitoes are less obtrusive than their cousins, the Anopheles mosquitoes, which carry malaria (responsible for 435,000 deaths in 2015), but are no less of a problem, and are now present almost everywhere in the world – including on French soil, with Aedes albopictus found in mainland France and Aedes aegypti in the overseas territories and departments on the American continent.
"However, in our imagination, Zika is the disease that most strikes fear into our hearts. This is because we have been shocked by images of two of its consequences:
– Progressive, generalized paralysis with Guillain-Barré Syndrome.
– The irreversibly tiny heads of babies born to women who contracted the Zika virus during pregnancy."
Erik Orsenna, Géopolitique du moustique, Ed. Fayard.

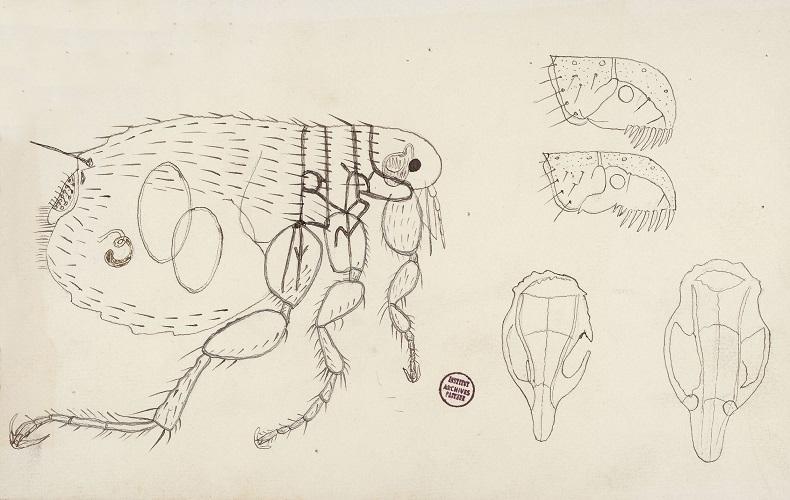
Images of mosquitos and other insects
Aedes albopictus (the tiger mosquito), Aedes aegypti, but also anopheles, tsetse flies and other bugs... a selection of entomological images from the Institut Pasteur Photothèque.

Vector-borne diseases are among the leading causes of morbidity and death in humans and animals.
Is the Zika virus more virulent now than it was previously?
In theory no. It's more a case of epidemic scale. The more sufferers there are at any one time, the higher the number of extreme cases. In addition, these extreme manifestations affect babies and pregnant women, which puts them in the media spotlight. So we find ourselves shocked at the 4,000 cases of microcephaly attributed to Zika. But we should also remember that there are between 30,000 and 50,000 deaths from dengue.
With Aedes albopictus and Aedes aegypti gaining ground, why does an outbreak not automatically follow, particularly in Europe?
Several factors come into play. Firstly, the hotter the climate, the faster viruses multiply. Mosquitoes become more contagious. Tropical regions are therefore more susceptible than temperate regions. Also, in hotter regions people live very much out of doors. It logically follows that they are in greater contact with mosquitoes, which are mainly active in the early morning and at twilight. Socio-economic levels also have an impact. A lack of mosquito eradication services encourages mosquito proliferation. This allows albopictus and aegypti – which love to breed in little nooks and crannies – to establish any number of larvae breeding grounds in badly maintained urban areas. Lastly, the higher the population density, the more quickly disease spreads.
The conditions in Europe do not favor an outbreak. However, we do know that the tiger mosquito is established in the south of France. We therefore need to be vigilant, as we have some concerns about what will happen when eggs start to hatch in May.
What strategies are planned to eradicate these mosquitoes?
The main problem is that Aedes albopictus and Aedes aegypti have developed resistance to insecticides. We therefore need to explore other avenues. One of these is to wipe out the mosquitoes. For example, we can irradiate males in order to render their sperm inefficient, so that they are unable to reproduce. We can also genetically modify them to make them dependent on an antibiotic. This means that, their progeny being similarly dependent, they will die out because the antibiotic is unavailable in their habitat. Lastly, there are small-scale trials in progress involving mosquitoes that carry a bacterium harmless to humans but which prevents mosquito eggs from hatching. The key limit of all these techniques is that nature dislikes a vacuum, and so destroyed populations are replaced by others. For example, on Reunion Island, aegypti has been eradicated from towns but albopictus, which had hitherto been contained in forest regions, took its place.
This is why we are studying a way to render mosquitoes incapable of transmitting the virus. The idea is to stimulate their immune system so that viruses are destroyed before reaching saliva and reproductive cells. Of course, it is always possible that they will counter this attack. It comes down to an arms race between the virus and the mosquito.
Rapid reproduction well suited to unfavorable conditions

Like all other mosquitoes, albopictus and aegypti reproduce quickly and easily. If the temperature is favorable when the female matures, she mates. Although like the male she feeds on vegetable saps, in order to reproduce she needs to feed on blood. For this reason she is known as hematophagous. Once she has bitten an animal or human, she goes off in search of a humid habitat in which to lay her eggs. Some mosquitoes like wide open spaces, such as the edges of lakes or rivers, but albopictus and aegypti prefer to lay their eggs in smaller larvae breeding grounds, such as holes in trees, flower-pot saucers, tires and such like. The eggs transform progressively into larvae, pupae and then mosquitoes. This development is possible only if they are submerged in water. Lack of water is fatal to the progeny of some species, but albopictus and aegypti can adapt to this situation. Their eggs can lie dormant in dry conditions for several months without hatching. A day or two after a return to damp conditions they resume their normal cycle, which lasts from 10 to 15 days. Once it reaches the adult stage, a mosquito will live for a period of between three weeks and three months. Given that a female lays 100 to 200 eggs every five days, half of which will produce female mosquitoes, albopictus and aegypti have unrivaled colonization abilities.
The long history of medical entomology
Medical and veterinary entomology is a holistic science. Very early on in the history of human society, people became aware that there was a link between insects, diseases and health. Today's entomologists, distant heirs of Aristotle, are required to take a new approach to these "vectors" by placing them in a historical, medical, socio-economic and environmental context and drawing on a wide range of complementary disciplines, from taxonomy to public health.
By Didier Fontenille, IRD Director of Research and Director of the Institut Pasteur in Cambodia, Vincent Robert, IRD Director of Research, and Gérard Duvallet, Professor at Paul Valéry University of Montpellier.
A MOOC on Medical entomology at the Institut Pasteur
In keeping with its mission to disseminate knowledge, the Institut Pasteur provides training programs such as the Medical Entomology MOOC, which focuses on insects and arthropods affecting human health and the associated diseases (malaria, dengue, Zika, etc.). This MOOC is coordinated by two medical entomologists, Anna-Bella Failloux from the Institut Pasteur, and Vincent Robert from the French Research Institute for Development (IRD) in partnership with the French National Conservatory of Arts and Trades (CNAM). The latest MOOC took place in February and March 2017.
Want to know more? Would you like to have a better understanding of mosquitoes? You can find the videos from this MOOC on the Institut Pasteur's YouTube channel. Don't forget to activate the subtitles in your player if necessary.
Well-traveled mosquitoes
"Aedes aegypti landed in North America's cotton plantations, and among the sugar cane fields in the Caribbean and Brazil, and subsequently adapted to a number of different environments. Aedes albopictus later left Asia, where they originated, probably around 1980 in a consignment of old tires that was shipped to Texas or New Mexico in the southern United States."
Erik Orsenna, Géopolitique du moustique, Ed. Fayard.
Originally, Aedes aegypti lived in the African forest and Aedes albopictus in Asia. In order to reproduce, females fed exclusively on animal blood – in particular that of monkeys – until humans came to live in their habitat. This invasion prompted them to adapt genetically. They became partly anthropophilic. Deforestation subsequently brought about their mutation. In the face of a shrinking habitat and food sources, the mosquitoes were driven into the towns. Some lines of Aedes aegypti became exclusively anthropophilic, whereas Aedes albopictus retained its more varied tastes. Over time, international trade, combined with the ability of Aedes mosquito eggs to lie dormant in dry conditions, encouraged their spread around the world. Aegypti first colonized Asia and then South America. Albopictus made the journey in reverse. Both have now colonized Europe, due in particular to a lack of mosquito eradication programs in certain countries. Albopictus is present in the south of France and moving north, while aegypti is moving east from Turkey and Georgia."

"It's little comfort when Didier [Fontenille], the director, assures me that we'll be completely safe if we're shipwrecked: no cases of schistosomiasis have ever been recorded in the area. However, some greater power preserved us from a watery grave – spirits, perhaps, or the Institut Pasteur logo adorning the door of our 4x4…"
Erik Orsenna, Géopolitique du moustique, Ed. Fayard.
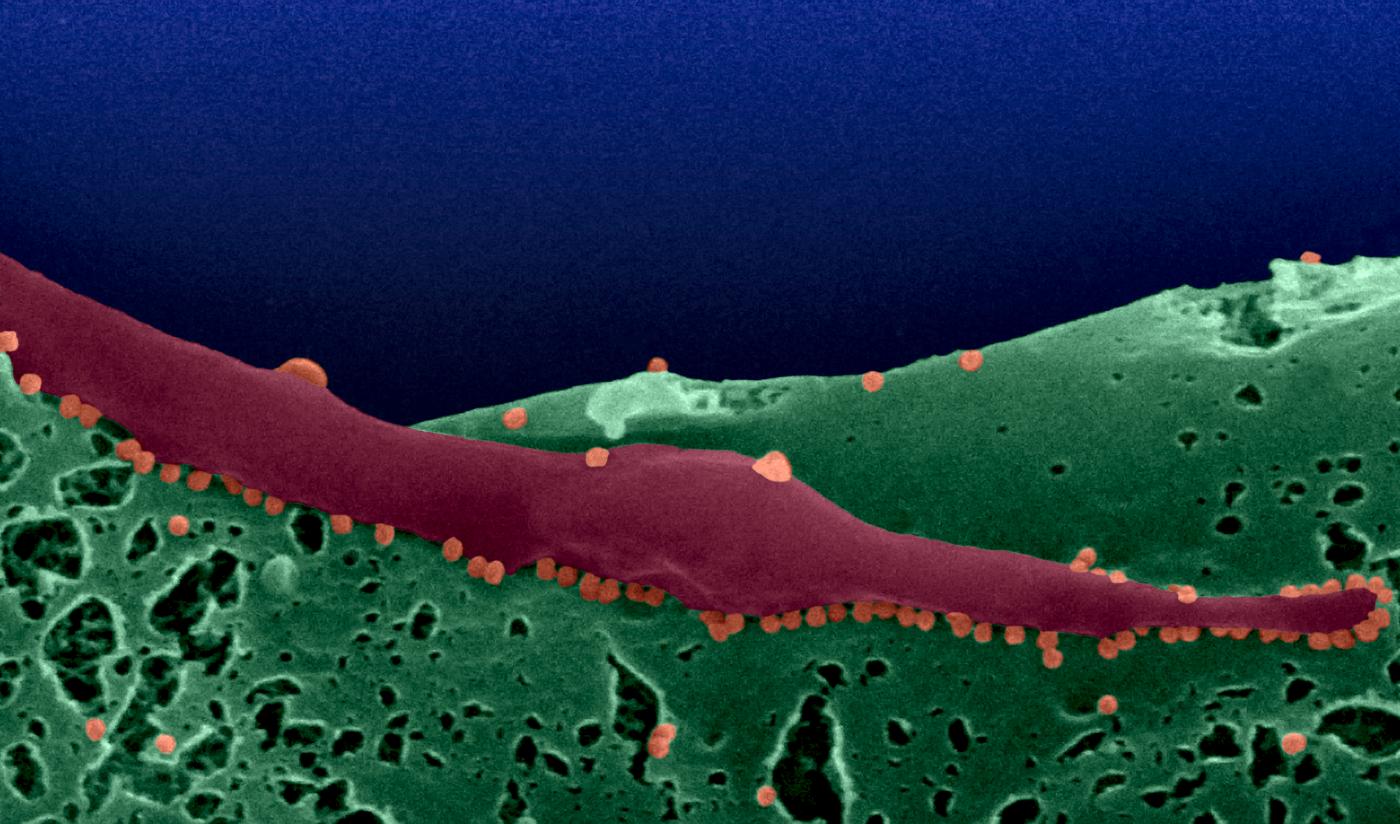
Viruses adapted to their hosts
During their various migrations, albopictus and aegypti mosquitoes do not travel empty-handed; they are potentially carriers of disease. When a female albopictus or aegypti bites a monkey or a human infected by a virus, she ingests the virus. If it is the HIV or flu virus, she digests it and it is killed. However, a genetic program protects Zika, dengue, chikungunya and yellow fever from the immune system of aedes mosquitoes, and these viruses are able to leave the insect's stomach intact. They then spread throughout the entire organism, reaching the saliva and reproductive cells, which both offer means of propagation. Firstly, when the female bites a new animal or human, she transmits the virus via her saliva. Secondly, every time she lays, just under 1% of her eggs will carry the virus. In addition, scientists have observed that the same mosquito may carry more than one type of virus, for example dengue and chikungunya, and can transmit them together in a single bite. Lastly, these viruses remain in mosquitoes throughout their entire lifetime.
In the face of these formidable vectors, prevention and control are based in part on reducing the number of mosquitoes at source, and in part on research into vaccines and diagnostic products. This is the basis of the arsenal deployed by the World Health Organization (WHO) against Zika within the framework of a worldwide strategic response. The potential destructiveness of Zika is not yet fully clear and, given the capacity of Aedes albopictus and Aedes aegypti to propagate and resist traditional mosquito eradication methods, scientists are focusing their efforts on combating the effects of the virus.
Chikungunya – a highly debilitating disease
Chikungunya is not a killer, but it is debilitating and may have sequelae. For a long time it was an uncharted disease, but in recent years outbreaks have become more common as the populations of its mosquito vectors have increased.
Chikungunya is caused by a virus in the Togaviridae family and is transmitted via Aedes albopictus and Aedes aegypti mosquitoes. The name "chikungunya" comes from Makonde, a language spoken in Tanzania and Mozambique; it means "walking bent forward", which is a reference to one of the symptoms of the disease.
And with good reason. Although often the infection goes unnoticed, when it does manifest symptoms it is a highly debilitating disease. Following an incubation period of 2 to 10 days, there is fever and joint pain, usually in the wrists, fingers, ankles, feet, knees and sometimes also in the hips and shoulders. These symptoms are combined with severe muscle pain, a skin rash on the torso and limbs, swelling in one or more cervical lymph nodes and conjunctivitis. Most symptoms disappear after a few days. However, joint pain, which is very debilitating, may persist for several weeks or may be chronic for years in some patients.
Since the early 2000s chikungunya has affected millions of people each year.
In 2007 transmission of the disease was recorded for the first time in Europe, in Northeast Italy.
At the Institut Pasteur
The Institut Pasteur's reaction to chikungunya, right from the start of the outbreak in 2005, is a clear demonstration of the ability of its scientists to take action and provide a swift response. This was the point at which the Institut Pasteur launched a wide-ranging program of research into the chikungunya virus. There are still ten teams* dedicated to studying the disease. Amongst other aspects, these teams are studying the immune-evading tactics of the chikungunya virus in response to anti-viral defense mechanisms in host cells and the ability of mosquitoes to transmit chikungunya to humans, as well as a molecular diagnostic tool. In parallel, a vaccine candidate against chikungunya is currently being developed.
* Teams led by Philippe Desprès, Frédéric Tangy, and Anna-Bella Failloux
A Task Force for responding to outbreaks such as Zika
Emerging and re-emerging infectious diseases are a threat to public health, as we saw with SARS in 2003, the influenza (H1N1pdm09) pandemic in 2009, MERS-CoV in 2012, and Ebola in West Africa in 2013, and as we are currently witnessing with Zika on the American continent. Frequent travel and increasing global economic interdependence have only served to add to the complexity of managing such threats. The Outbreak Investigation Task Force is the Institut Pasteur's response to outbreaks of emerging and re-emerging infectious diseases.
Text by Arnaud Fontanet, director of the Center for Global Health (CGH).
Yellow fever still active
Yellow fever is caused by the Amaril virus, and is an acute hemorrhagic disease transmitted by Aedes mosquitoes. The name "yellow fever" refers to the jaundice present in some patients. Although a vaccine has been available since 1932, yellow fever is still a widespread killer in the 21st century. Annual global cases of yellow fever are estimated at 200,000, and deaths from the disease at 30,000.
The disease is not always severe. Following an incubation period of a week, symptoms start with a fever, chills, muscle pain and headaches. Symptoms are flu-like, but also resemble those of dengue or malaria, which means that diagnosis can be difficult. In general, sufferers start to recover after three or four days.
However, according to WHO, 15% of sufferers go on to develop a much more serious form just as they are starting to feel better. In addition to a high fever, there is vomiting, along with bleeding disorders, the jaundice that gives the disease its name, and renal failure. Half of these patients die within 10 to 14 days, after a phase of delirium, convulsions and coma. Rest, the administration of drugs to reduce fever, vomiting and pain, and rehydration therapies are the only methods of treating this disease. Vaccination is the main preventive measure against yellow fever (see the recent research journal news article Yellow fever: using modeling to optimize the use of vaccine stocks). The yellow fever vaccine is safe, affordable and highly efficient. A single dose is enough to confer lifetime immunity from the disease. The Institut Pasteur in Dakar alone produces all the doses required by WHO for administration in Africa.
Yellow fever is currently endemic in 47 American and African countries that are home to 900 million people. Monitoring, along with intensive vaccination campaigns – both preventive and when there is a local diagnosis – are successful in limiting outbreaks. Between 2007 and 2014, 14 African countries started or successfully led yellow fever vaccination campaigns.
At the Institut Pasteur
Three Institut Pasteur units are particularly involved in yellow fever research: the Flavivirus-Host Molecular Interactions Unit (led by Philippe Desprès), the Immunobiology of Dendritic Cells Unit (led by Matthew Albert) and the Structural Virology Unit (led by Félix Rey). Yellow fever is also the subject of research carried out by the Institut Pasteur International Network, in particular at the Institut Pasteur in Dakar, Senegal.

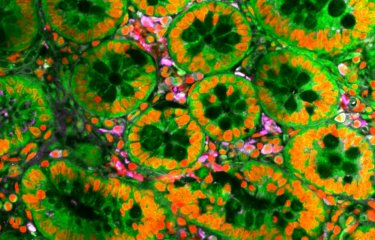
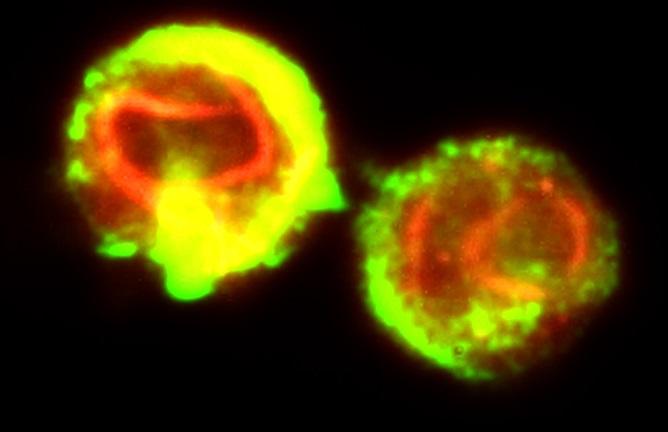
Genitalia of a male Culex pipiens mosquito, with forceps, viewed by scanning electron microscopy. Colored image. West Nile vector.
©Institut Pasteur/Christine Schmitt, Ultrastructural Microscopy Platform- Anna-Bella Failloux Arbovirus and Insect Vectors Laboratory. Colorisation Jean-Marc Panaud.
Rabies in Cambodia
As part of his trip round the world to gain a better understanding of mosquitoes and write his book Géopolitique du moustique (The Geopolitics of the Mosquito), published by Fayard, Erik Orsenna made a stop in Cambodia. He visited the Institut Pasteur in Phnom Penh. This was the chance for him to discover that, in addition to vector-borne diseases, rabies is a neglected disease that is still rife in this country. The Cambodian population suffers nearly 600,000 severe dog bites each year. The following is a review of rabies in Cambodia by Didier Fontenille, who heads up this institute in the Institut Pasteur International Network.
Rabies in Cambodia, by Didier Fontenille, director of the Institut Pasteur of Cambodia.
"The Geopolitics of the Mosquito" according to Erik Orsenna
Erik Orsenna, writer, member of the Académie Française and ambassador for the Institut Pasteur, is publishing his new book Géopolitique du moustique, Petit Précis de Mondialisation IV, published by Fayard, which will be on sale in bookshops from April 3, 2017.
Erik Orsenna.